It’s a topic that comes up numerous times in my coaching group. I also see women commenting about it on the comments section of my advertisements. Hundreds of emails over the years have also alerted me to the itching, sneezing, wheezing and food and alcohol intolerances, of menopausal and post-menopausal women.
If it’s the same for you, then I’m not surprised. Menopause changes our immune response and it’s all to do with histamine levels.
If you’ve ever had a glass of red wine and started sneezing, or your asthma has become worse in menopause, or you have itchy skin, or runny tearful eyes, then you need to know about the role of histamine and how this changes with age.
Histamine is an important component of our immune system because it moderates inflammatory responses in the body.
In the early phase of any inflammatory response, histamine is released from mast cells. The majority of these mast cells reside in the gut, but there are also numerous mast cells in the skin, uterus, adrenal glands and for those who sneeze a lot, also in the nasal cavity.
When mast cells detect a substance that triggers an allergic reaction (an allergen), they release histamine and other chemicals into the bloodstream. Histamine makes the blood vessels expand and the surrounding area itchy, swollen and inflamed. This could be outside your body on your skin, or inside your body in your organs. Mucus might also build up in the airways, which become narrower causing sneezing or asthma-type wheezing. When this type of reaction occurs, this is known as histamine intolerance.
However, here’s the kicker for all of us as we transition menopause. Both oestrogen and progesterone receptors are on these mast cells too.
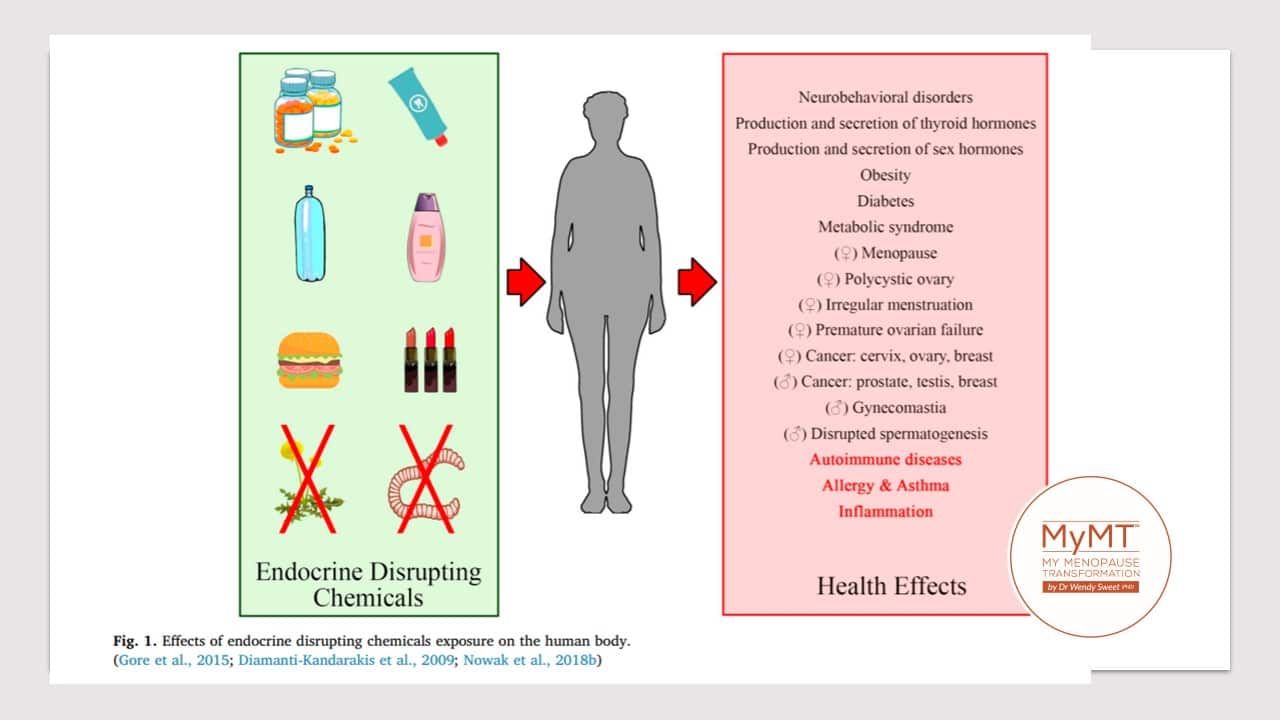
This is why menopause hormonal changes impact the release of histamine from mast cells in response to compounds which stimulate an allergic reaction in the body – and when oestrogen-mimicking hormone disruptors attach to these mast cells as well, the result is an allergic reaction – from sneezing, to scratching to hot flushes, leaky gut syndrome, fibromyalgia or shortness of breath – all signs that you are reacting to ‘something’ in your food, fluid, or environment.
In my coaching group this week the focus has been on gut health and how to change this back to normal in 21 days – the evidenced time to turn around leaky gut syndrome for most women.
One of the things I’ve been suggesting to women is to understand how, changing to organic produce for their fruits and vegetable intake if possible, can make a big difference to not only their gut and liver health, but also their immune health. This is because new research is emerging about the effect of hormone disruptors in certain foods, chemicals and sprays which can cause havoc with our immune system as we move through menopause and into post-menopause. With a powerful connection between gut health, liver health and our immune response, this is important for women to understand.
Different phases of the female menstrual cycle are known to affect histamine release from mast cells. Peak oestrogen levels correlate with the nasal mucosa becoming hyper-reactive and hyper-sensitive to histamine. This is why, during peri-menopause and as you transition into menopause, your symptoms may change according to your menstrual cycle.
When the release of histamine is out of balance, we become prone to chronic low-grade inflammation – also associated with ageing. With the increased presence of chronic inflammation, comes more release of histamine into the circulation and for some of you, there is histamine intolerance and a range of allergies that may suddenly appear in mid-life.
Histamine intolerance is the consequence of excess levels of circulating histamine causing a range of symptoms that you don’t necessarily relate to menopause hormonal changes.
Some reactions in women are more severe than others, and scientists now know that there may be other influences as well, including:
- Low Vitamin B6 (absorption can be reduced by antibiotics and hormonal contraceptives).
- Low Vitamin C
- Copper deficiency
- Low Vitamin D
- Eating foods that contain high levels of histamine e.g. fermented foods such as sauerkraut, processed meat, dried anchovies, fish sauce, spinach, tomatoes, eggplant, fish, chicken, yoghurt, soy, red wine.
- Eating foods that induce increased histamine release from mast cells – pineapple, bananas, strawberries.
- Eating foods that are high in preservatives, additives and/or chemical sprays.
- Stress, both acute and chronic (which also impacts the gut mucosa) may increase the circulating levels of histamine.
- Poor gut health.
Turning around your histamine intolerance means factoring in all of these connections and exploring what you may be sensitive to, whether this is food, alcohol, chemicals, additives, preservatives, stress or the fact that you are oestrogen dominant, as I used to be too.
As my knowledge grew about the role of inflammation on our symptoms in menopause, I began to look at the life-course context in which we have lived our lives and this bought me to the effect of all the environmental toxins that have arrived over the past 40 years … our generation.
Professor Garry Egger used to present at many health and fitness conferences that I’ve attended over the years. His research work is now positioned in obesity research as well as inflammation and ageing research. In his presentations, Professor Egger often discuss the factors that contribute to inflammation in our body – in our liver cells, fat cells, joints and muscles and in our gut. Many of these inflammatory changes, he suggests, have begun with increased exposure to environmental toxins over the years.
His research has shown that the role of pesticides, herbicides and household chemicals, are equally important to consider removing from our diet. These substances over our lifetime contribute to ‘Inflammaging’ – a term which describes the inflammatory changes occurring in our cells and tissues with age – gut cells are also becoming inflamed.
Professor Egger also confirmed my belief that modern medicine is not taking a ‘whole body’ approach to turning around inflammation. Inflammatory changes can accelerate in midlife. I talk about this in my Masterclass on Menopause.
As Professor Egger mentions, “As Doctors, we have been operating in silo’s. We haven’t been taking into account all of the other factors leading to meta-inflammation which is linked to many chronic diseases as we age.” As such he has been leading research into ‘Anthropogens Theory’ over the past few years – which he defines as ‘An inflamed body living in an inflamed man-made environment.’ [Egger et al., 2015].

Liver health is important obviously for clearing toxins, as are your Vitamin D levels (this affects mast cells in your skin) and reflecting on what you react to. Because of the number of mast cells in the nasal cavity, then I would suggest that (re)learning to nasal breathe is important to help to reduce the hyper-activity and inflammation of your nasal nerves. Your water intake will also be important.
As always though, please see your medical specialist if your allergy symptoms are overwhelming you. There are lots of treatments available these days as well as better knowledge about histamine-reduction dietary approaches, which may help in the short-term. The histamine content of foods can vary significantly – for example, freshly caught fish contains almost no histamine, whilst the histamine content of cured, pickled or not really fresh fish can me more than 2,000mg/kg. [Reese, 2018].
The histamine content of cheese, another frequently cited histamine-rich food, can also vary significantly. Emmental cheese, Swiss mountain cheese or Blue cheese, contain less than 5mg/kg of histamine compared to other types of cheeses. But as studies report, even the detailed knowledge of the histamine content of certain foods cannot be solely attributed to histamine intolerability. [Reese, 2018]. I tend to agree. For example, if food is the only factor explored in histamine intolerance, this leaves out the role of hormones on the activity of our mast cells as well as the changes occurring in our immune system, including our gut health changes as we move through menopause.
If women deal with these, as well as their sleep concerns, and change their nutrition and lifestyle to accommodate their hormonal changes (such as learning to say no to red wine and find an alternative drink instead as my friend and I had to do!), then it’s amazing how many of our intolerances go away – as well as our weight gain. Teaching you how to do this and supporting you whilst you are doing it, is the essence of my 12 week coaching programmes, which you can read about on the website and listen to my videos there as well.
Sometimes we feel so ‘stuck’ when it comes to our symptoms and what it all means and many of us end up believing that we are destined for an unhealthy ageing as a result because we can’t get adequate answers to the numerous symptoms that don’t quite fit the realm of ‘menopause symptoms‘ – including the arrival of unexplained allergies. But as I’ve found and thousands of other women who join me for a few months, it doesn’t have to be this way at all.
Can I help you with your symptoms and/or your weight gain?
If you are struggling with your mid-life weight, health or symptoms, then come on board if you can into my 12 week online programmes. Or as a starting point, you can purchase my online Masterclass on Menopause. This is only NZ$15 (approx. AUS$14 or UK£7.5). I hope you can join me in this powerful 2 hour webinar. The great news is that now you can watch it anytime, anywhere and even pause it whenever you like and go and make yourself a cuppa too.

References:
Blasco, M.P., Chauhan, A., Honarpisheh, P. et al. Age-dependent involvement of gut mast cells and histamine in post-stroke inflammation. J Neuroinflammation 17, 160 (2020). https://doi.org/10.1186/s12974-020-01833-1
Egger G, Colquhoun D, Dixon J. “Anthropogens” in Lifestyle Medicine. (2015). American Journal of Lifestyle Medicine. 9(3):232-240. doi:10.1177/1559827613512596
McCarthy M, Raval AP. The peri-menopause in a woman’s life: a systemic inflammatory phase that enables later neurodegenerative disease. J Neuroinflammation. 2020 Oct 23;17(1):317. doi: 10.1186/s12974-020-01998-9.
Nowak, K., Jabłońska, E., Ratajczak-Wrona, W. (2019). Immunomodulatory effects of synthetic endocrine disrupting chemicals on the development and functions of human immune cells. Environment International, 125, 350-364. ISSN 0160-4120.
Reese I. (2018). Nutrition therapy for adverse reactions to histamine in food and beverages. Allergologie select, 2(1), 56–61. https://doi.org/10.5414/ALX386
Shah S. (2012). Hormonal link to autoimmune allergies. ISRN allergy, 2012, 910437. https://doi.org/10.5402/2012/910437

