2/3 of those on antidepressants in the UK, NZ and Australia are female, and typically in their 50s and 60s.
Why is depression so prevalent in women? This was a question posed by researchers in Canada (Albert, 2015) and one that I have often thought about too. But not just any women – those in mid-life.
The prevalence of major depression is higher in women than in men and here in New Zealand, we are in the top-10 of countries to have the highest rate of antidepressant use in the western world. It is higher in women and the rate of prescriptions increases with age. (Bowden, Gibb et al, 2019). Serious stuff.
I was offered antidepressants myself. At the time, I had no idea that going into menopause was a vulnerable time for my mental health.
However, I was curious as to why, when I have no history of depressive incidents nor post-partum depression (both factors in menopause-related depression), as to why I not only felt emotionally all over the place, but why my Doctor wanted to put me on them.
Since setting up MyMT™, I’ve read hundreds of pre-entry screening forms, where women indicate that they are taking HRT, Bio-identicals, Anti-depressants and anti-anxiety medications for their menopause symptoms.
Whilst I never interfere in this with women because these are all powerful medications that need to be monitored by their medical specialists, what intrigues me the most is that they still report experiencing hot flushes, insomnia, anxiety, brain fog and depression.
It doesn’t go past me that these medications are not necessarily working for them, especially as they move into post-menopause. I became curious as to why.
The conclusion I come to time and time again, is that menopause symptoms aren’t being looked at through the lens of our biological ageing. I’m not just talking about our changing reproductive hormones either.
There are numerous physical changes that go on inside our body at this time too. These changes occur when oestrogen and progesterone naturally decline and exert influences on the deep tissues and cells that make up every structure in our body. This includes our digestive system and colon.
For millions of women around the world, menopause means poor sleep, hot flushes, worsening anxiety, brain fog and feelings of depression. But there’s also another symptom that isn’t often associated with menopause, nor is it associated with menopause-related anxiety, depression and foggy brain.
And that’s the changing health of the gut and digestive system during menopause.

So, do your client’s suffer from Irritable Bowel Syndrome (IBS)? Or diverticulitis? Or do they swing between being constipated and having diarrhea? Maybe their brain feels foggy all the time and they find it difficult to concentrate?
And perhaps these changes have arrived during their menopause transition and they have no idea that these changes to the microbiome might be related to their feelings of melancholy?
At least 50% of women in my coaching programs tell me that they are experiencing gut health issues that have mainly arrived since they went into their menopause transition. Unbeknownst to many of them, their changing gut health impacts their anxiety levels and brain fog too.
I have Australia’s Professor Rosemary Stanton to thank for my lightbulb moment.
“After 4 generations of a low-fibre diet since modern food processing arrived in the 1960’s & 1970’s, the gut microbiota has changed to the extent that it no longer supports our immune health. Never before have we seen so much chronic disease caused by the western diet. Diversity in vegetables has the single greatest influence on the gut microbiota. The Mediterranean way of eating is the way to turn this all around.”
The link between changing oestrogen levels and gut health could well be the cause of your menopause bloating, IBS or leaky gut and menopause-related depression.
Knowledge of the gut-brain connection has increased 10-fold over the past decade. This has been due to improved brain research as well as genetic research. Both have opened the door towards understanding gut health and the link to disease, especially the effect of the accumulation of inflammatory changes as we get older.
The gut microbiome is one of the largest organs in the body (along with the skin) but here’s what blew me away – when I attended the Australasian Society of Lifestyle Medicine conference late last year, researcher, Professor Thomas Borody, reported that the gut is responsible for producing 70% of the body’s energy.
Can you imagine what happens to your client’s energy levels, sleep, health and moods, when their gut isn’t performing to its best?

What is the gut microbiome and why does it matter to in menopause?
The microbiome is the community of bacteria and other microbes that live in the gut and elsewhere in our body. Researchers now understand that there is an important connection between the human gut microbiome and the brain.
“The connection between the brain and gut is because messages are sent up and down the vagus nerve – the major nerve that runs from our brain to our heart, stomach and intestines. The vagus nerve therefore, has a profound influence on the gut microbiota as well as pro-inflammatory markers.
The reason for this, is because the vagus nerve transfers stress cytokines (inflammatory markers) between the gut and the brain. So, stress is the ‘hammer’ which acts on the brain and the gut. When we keep activating our stress response, then this increases the ‘leakiness’ of the gut. When the gut is leaky, we lose the ability to absorb the nutrients we need for our health and this increases oxidative stress in the body.” [Professor Zoltan Sarnyai, 2019)
When women aren’t sleeping the gut isn’t healing properly overnight, pockets of inflammation may accumulate throughout the digestive system.
Add to this, the changes to food and chemical environments over the decades as well as increasing exposure to medicines, then it’s no surprise that women may develop worsening gut health in midlife, which may affect their moods and melancholy.
Other changes may occur too. Enzymes that break down food, slowed peristalsis (gut motility) and changes to liver function (we produce less bile to break down fats), also are a hallmark of menopause and age-related changes.
As well, for those of your clients who are high-volume exercisers and/or under a lot of stress, then their body may remain in ‘fight or flight’ mode. This causes the vagus nerve to be stimulated more often.
The Thyroid Gland Matters to Gut Health:
The thyroid gland produces hormones that are integral to the function of the gut microbiome and the brain.
If your clients do have a digestive disorder, such as Irritable Bowel Syndrome or Diverticulitis, then this inflammation disrupts function in the gut. In turn, the inflammatory changes to the gut, may also disrupt thyroid function. When the thyroid isn’t functioning as well as it should (both hypothyroidism and hyperthyroidism), this causes further disruption to moods, motivation and emotional state, via the HPA-Thyroid Axis.
For your menopausal clients, this HPA-Thyroid Axis and gut dysfunction, may present as increased anxiety, depression and brain fog. Hence, restoring gut health and helping clients to improve the gut microbiome is fundamental to reducing anxiety, brain fog, and/or depression.
3 Things You Can Do to Help your Client’s Manage their GUT HEALTH:
When we understand the powerful connection between the brain, the gut, the vagus nerve, existing gut inflammation AND menopause, then we need to focus on these three factors:
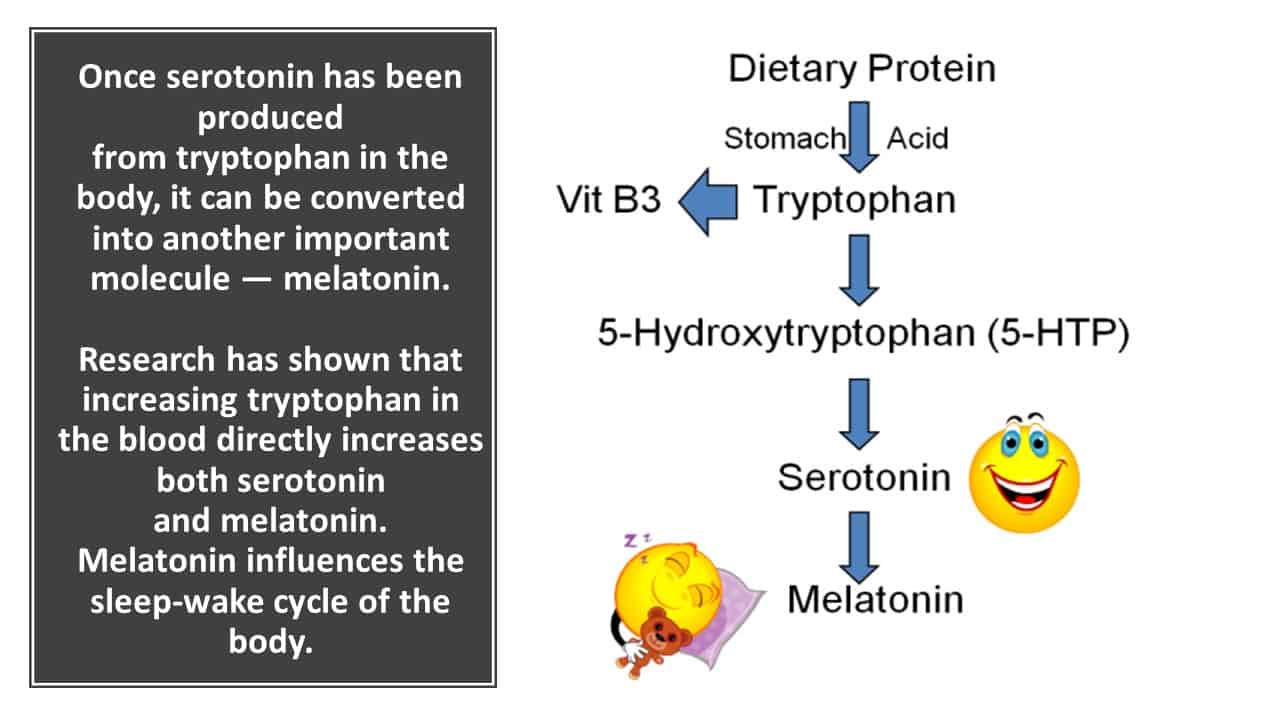
- Sleep All Night – as I keep saying to women, if you aren’t sleeping, then you aren’t healing and your heart rate stays higher during the day. The gut functions on a 24 hour circadian rhythm as do all of the major organs, so improving sleep, improves the gut and vice versa. This is why foods containing a protein called TRYPTOPHAN are important. Tryptophan increases serotonin production, which in turn, improves melatonin production.
- Help Clients to Improve their Food Quality and Vegetable Diversity –
Professor Rosemary Stanton of Australia has been studying the health of the population in Australia for over four decades now. As she stated at the conference – “The way to heal the gut is to have diversity in vegetable intake and increase fibre. This is what the gut has been designed for. Decades of low fibre, processed foods have resulted in worsening health of the population and a plethora of diseases which are mainly related to our changing food environment.”
The Iowa Women’s Health Study (2019) found a statistically significant association between fibre intake quartiles and validated Mental Health scores in menopausal and post-menopausal women.

3. Understand that, in order to heal, the gut must empty overnight. I encourage women as much as possible to allow their digestive system to rest for 12 hours overnight. This means that the timing of food and fluid is important. If women can avoid food for around 12 hours overnight (this changes obviously for shift-workers), then their digestive system gets the chance to actually digest and absorb the food that is eaten during the day.

A healthy gut microbiome is a diverse microbiome, which has a large number of bacteria. When women have a healthy gut, then this is fundamental to their mental and emotional health.
Whilst some clients may require medical and/or professional nutritional intervention for Gut Health, including a FODMAP diet, underlying any of these interventions should also be sleep, diet and exercise strategies that help to improve gut health as women move through menopause.
I talk about this aspect of menopause and lifestyle science in the MyMT™ Practitioner Course too – details are on the website.
References:
Albert P. R. (2015). Why is depression more prevalent in women? Journal of psychiatry & neuroscience : JPN, 40(4), 219–221.
Feraj, J. (2017). Micro-nutrients, depression and inflammation among women of reproductive age. Doctoral Dissertation 993, University of Massachusetts.
Freeman, E.W. (2015). Depression in the menopause transition: risks in the changing hormone milieu as observed in the general population. womens midlife health 1, 2. https://doi.org/10.1186/s40695-015-0002-y
Glezerman, M. (2016). Gender Medicine. Duckworth & Co Publ.
Graziottin A. & Serafini A. (2009). Depression and the menopause: why antidepressants are not enough? Menopause Int. Jun;15(2):76-81. doi: 10.1258/mi.2009.009021. PMID: 19465674.
Heitkemper, M., & Chang, L. (2009). Do fluctuations in ovarian hormones affect gastrointestinal symptoms in women with irritable bowel syndrome?. Gender medicine, 6 Suppl 2(Suppl 2), 152–167. https://doi.org/10.1016/j.genm.2009.03.004
Morimoto RI, Cuervo AM. Proteostasis and the aging proteome in health and disease. J Gerontol A Biol Sci Med Sci. 2014 Jun;69 Suppl 1(Suppl 1):S33-8. doi: 10.1093/gerona/glu049.
Mahmood Akbar, Pranoy Toppo, Aamir Nazir. (2024). Ageing, Proteostasis, and the Gut: Insights into Neurological Health and Disease. Ageing Research Reviews, 102504, ISSN 1568-1637.
Mulak, A., Taché, Y., & Larauche, M. (2014). Sex hormones in the modulation of irritable bowel syndrome. World journal of gastroenterology, 20(10), 2433–2448. https://doi.org/10.3748/wjg.v20.i10.2433
Nie, X., Xie, R. & Tuo, B. (2018). Effects of Estrogen on the Gastrointestinal Tract. Dig Dis Sci 63, 583–596.
Odamaki, T., Kato, K., Sugahara, H. et al. (2016). Age-related changes in gut microbiota composition from newborn to centenarian: a cross-sectional study. BMC Microbiol 16, 90. https://doi.org/10.1186/s12866-016-0708-5
https://www.researchgate.net/publication/322946988_Prevalence_of_Thyroid_Dysfunction_in_Irritable_Bowel_Syndrome
Sjöstedt P, Enander J, Isung J. Serotonin Reuptake Inhibitors and the Gut Microbiome: Significance of the Gut Microbiome in Relation to Mechanism of Action, Treatment Response, Side Effects, and Tachyphylaxis. Front Psychiatry. 2021 May 26;12:682868. doi: 10.3389/fpsyt.2021.682868.
Veira, A., Castelo, P. et al, (2017). Influence of oral and gut microbiota in the health of menopausal women. Front. Microbiol.
Related Tag: Menopause Treatment
Xu F, Xie Q, Kuang W, Dong Z. Interactions Between Antidepressants and Intestinal Microbiota. Neurotherapeutics. 2023 Mar;20(2):359-371. doi: 10.1007/s13311-023-01362-8. Epub 2023 Mar 7.

