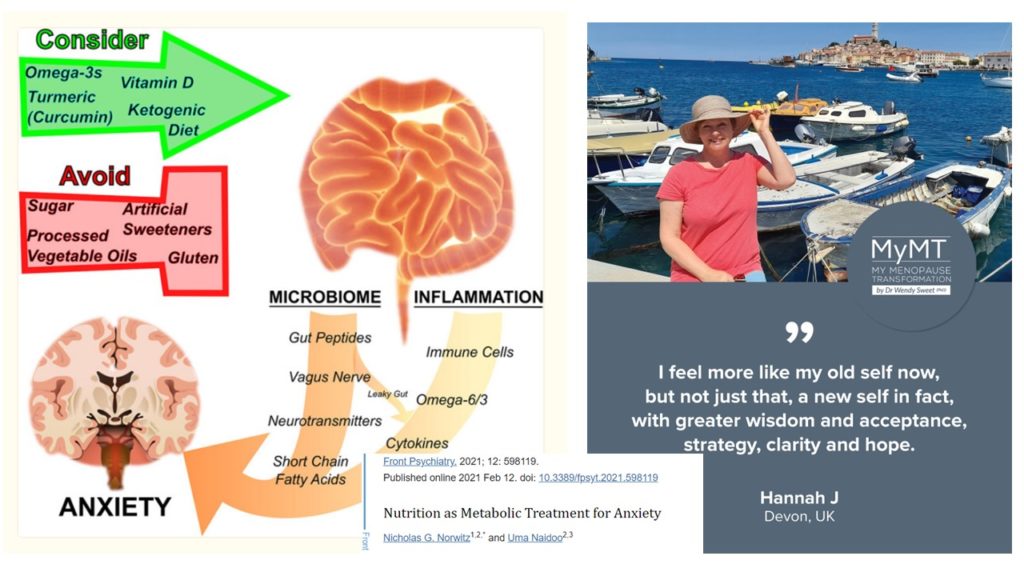
‘Despite the overwhelming prevalence of anxiety in modern society, medications often fail to achieve complete symptom resolution. We highlight the roles of the microbiome and inflammation as influencers of anxiety, and discuss the evidence base for specific nutritional interventions.’ [Norwitz and Naidoo, 2021]
Most of us know the feelings of anxiety don’t we? The elevated heart rate, holding our breath or breathing more rapidly, and the feeling that there is so much more to do in our day that we hurry from one task to another.
We talked about anxiety levels of women and this new study in my Health Practitioners zoom call this week.
Some of the Practitioners were presenting their case studies and one of them spoke about her client who was stressed and always busy – from early morning to night-time, she was active and busy. As her client hurried from one task to another, she told the Practitioner she didn’t have time to eat. Her food recall also suggested this as well. There wasn’t much written down. She mainly lived on soy lattes and cups of tea with sugar, as well as lots of supplements to try and reduce her hot flushes and induce her sleep.
But here’s the thing. Those menopause supplements weren’t helping, nor were they giving her the nutrients that her brain and nervous system needed to help reduce her anxiety levels. Nor was she eating enough fats and certain nutrients to not only give her the energy that she needed to get through her day, but to calm her anxiety levels as well as to reduce inflammatory changes that arrive with an over-stimulated gut.
Many of us forget that the gut bears the brunt of our anxiety and worry. Changes in the gut microbiome (dysbiosis) and inflammation with higher anxiety levels was a leading finding in the study I was sharing with the Practitioners.
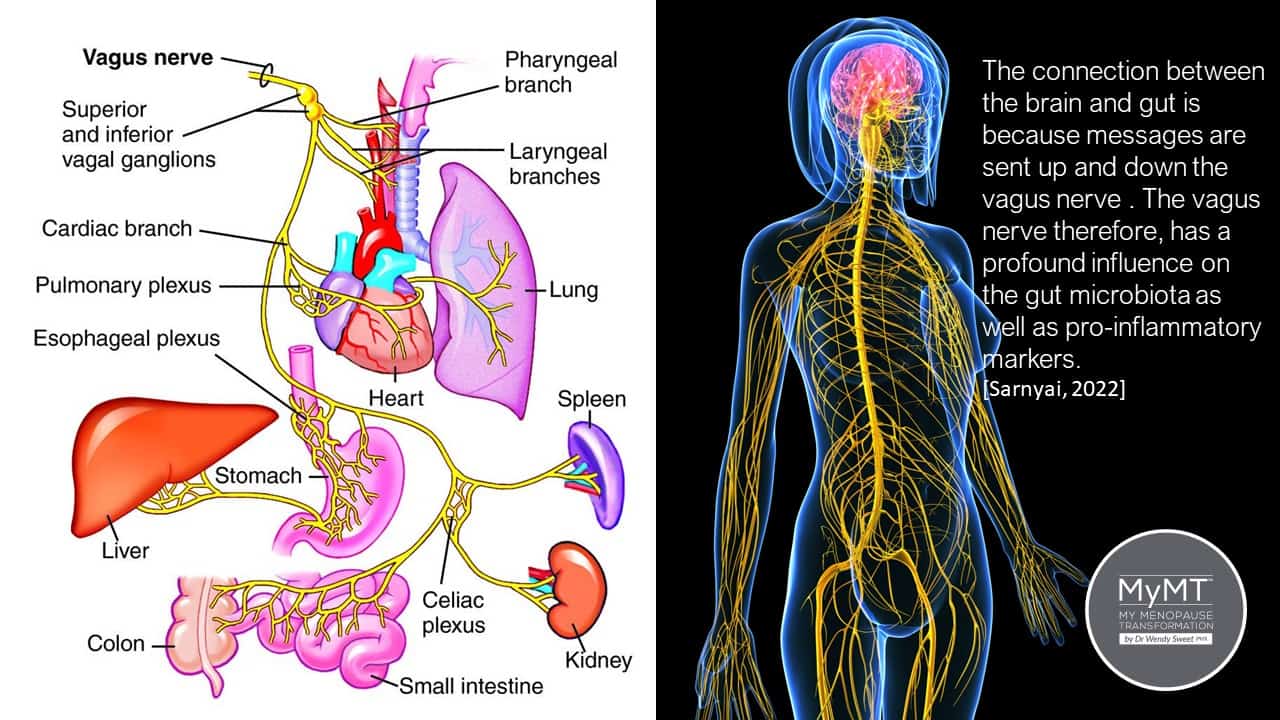
We all have various sources of worry and concern that cause us to become more anxious don’t we? However, as we arrive in our menopause transition, anxiety is heightened with the ageing of our nervous system and the decline of oestrogen on receptors situated on the outer sheath of the nerves. This also occurs on one of the longest nerves in the body – your vagus nerve.
The vagus nerve represents the main component of the parasympathetic nervous
system. As such it oversees a vast array of crucial bodily functions, including control of mood, immune response, digestion, and heart rate. (Breit et al, 2018). If you are experiencing increased anxiety, then you cannot ignore the vagus nerve, nor your gut health, nor the accumulation of inflammatory changes on your nerves.
It was back in the 1950s that those studying human anatomy and ageing changes, noted that ‘starting in the fourth decade of life and continuing into the fifth decade, there is an increase in connective tissue and a reduction in the patency of the blood vessels.
With this gradual reduction in blood supply and increase in connective tissue, there seems to be a gradual alteration and reduction of the nerve fibres, especially the larger ones. Beginning in the fifth decade of life, there is a continual decrease in conduction velocity (speed) in the nervous system.’ [Wilcox, 1956].
If you are feeling that your nerves are a bit wired and your anxiety levels are high, then please remember that because your oestrogen levels are declining and your nervous system is ageing, it’s time to slow down a bit with the pace of life.
Menopause, is the biological gateway to our ageing and when I began to explore the ageing research about all the changes that go on in our body as we move through menopause and into our older years, the evidence shared in much of this research went beyond the reproductive hormones. It helped me to move towards better understanding of the relevance of inflammatory changes that arrive in menopause and how we can mitigate these changes, thereby reducing our symptoms.
Chronic inflammation is a feature of numerous disorders and diseases of the neurological system, including anxiety. (Norwitz & Naidoo, 2021]. Hence, reigning in your anxiety levels takes more than pills. It also takes sorting out your nutrition as well as your gut health.
I never fully appreciated that arriving in mid-life would cause so many changes to our organs in the body – especially the nervous system. For decades, menopause conversations and interventions have primarily focused on the loss of our reproductive hormones in menopause – the master hormones from the pituitary gland (Follicle-Stimulating Hormone and Luteinizing Hormone) and oestrogen and progesterone.
But there’s more to this conversation too – and that is how our nervous system and brain are ageing and changing.
Your brain is part of your nervous system. It is the ‘mother-ship’ for your nerves and this is why our spinal column and every single nerve in the body comes off the base of our brain.
A typical day for most women is full of anxiety-inducing events. As we transition through menopause, the loss of oestrogen going to your oestrogen receptors throughout your nervous system compounds your feelings of anxiety and causes your heart rate to increase. Some of you will get more hot flushes, some of you will experience a heart rate that feels like it is ‘racing’.
As oestrogen and progesterone levels continue to decline as you pass into menopause and post-menopause, your nerves are ageing as is your brain. Both structures rely on oestrogen to help with nerve conduction. This is also why the addition of HRT helps many women feel calmer and reduces their anxiety levels. Some herbs do the same too and in the new research, turmeric (curcumin) gets a special mention as do other nutritional strategies which I share with you below.

Negative emotions can shift the microbial ecosystem in your gut by the release of stress hormones which impact the nerves which control our gut and digestive system.
As such, individuals suffering from anxiety disorders and other stress disorders exhibit elevated levels of inflammatory markers in the circulation, mentions Norwitz and Naidoo (2021). Whilst the mechanisms as to how this occurs very, the authors suggest that modulating and managing inflammatory changes in our gut which contribute to heightened anxiety disorders, require specific changes to the diet.
These changes include the following:
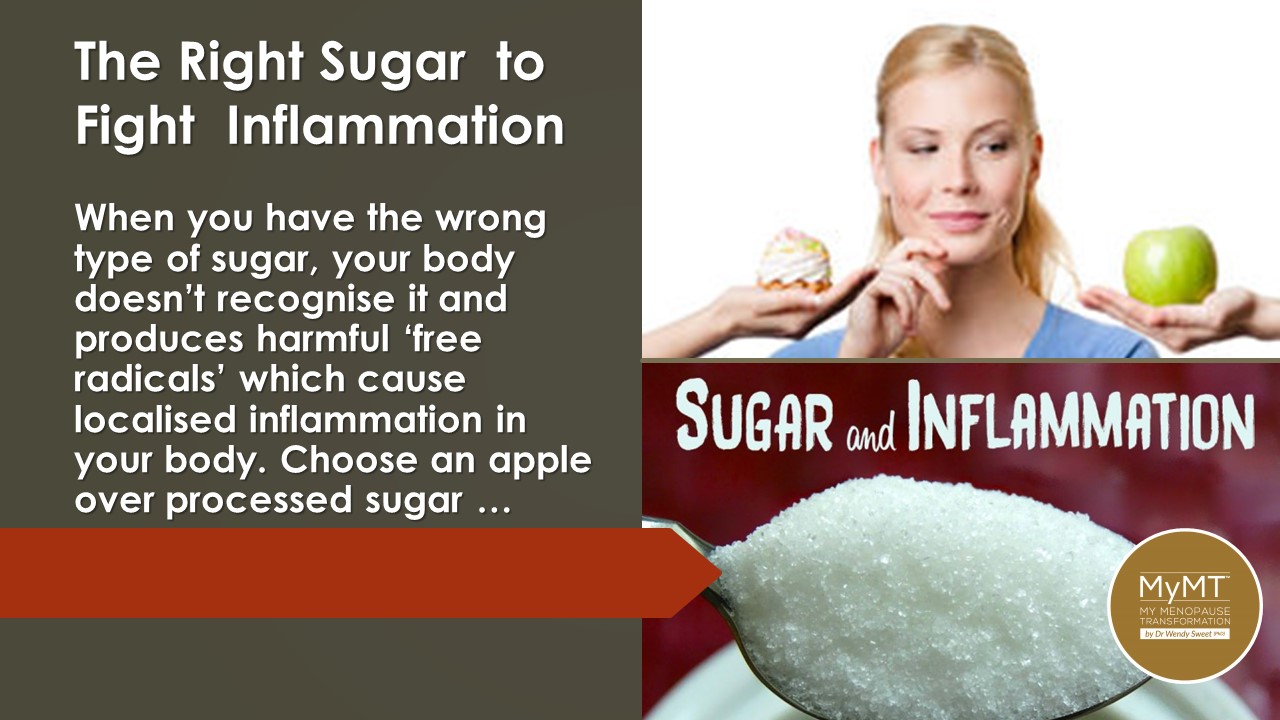
- Get off refined sugar, especially high fructose corn syrup. Sugar attaches to molecules throughout the body and can increase neuro-(nerve) inflammation.
- Remove artificial sweeteners from your diet. Administration of artificial sweeteners to animals have been known to increase anxiety through increasing the production and secretion of stress hormones. Aspartame in particular gets a mention, as it can block the transform of dopamine and serotonin precursors in the brain and can increase the levels of excitatory nerve transmitters. This, according to the authors (Norwitz & Naidoo, 2021) may contribute to heightened anxiety.
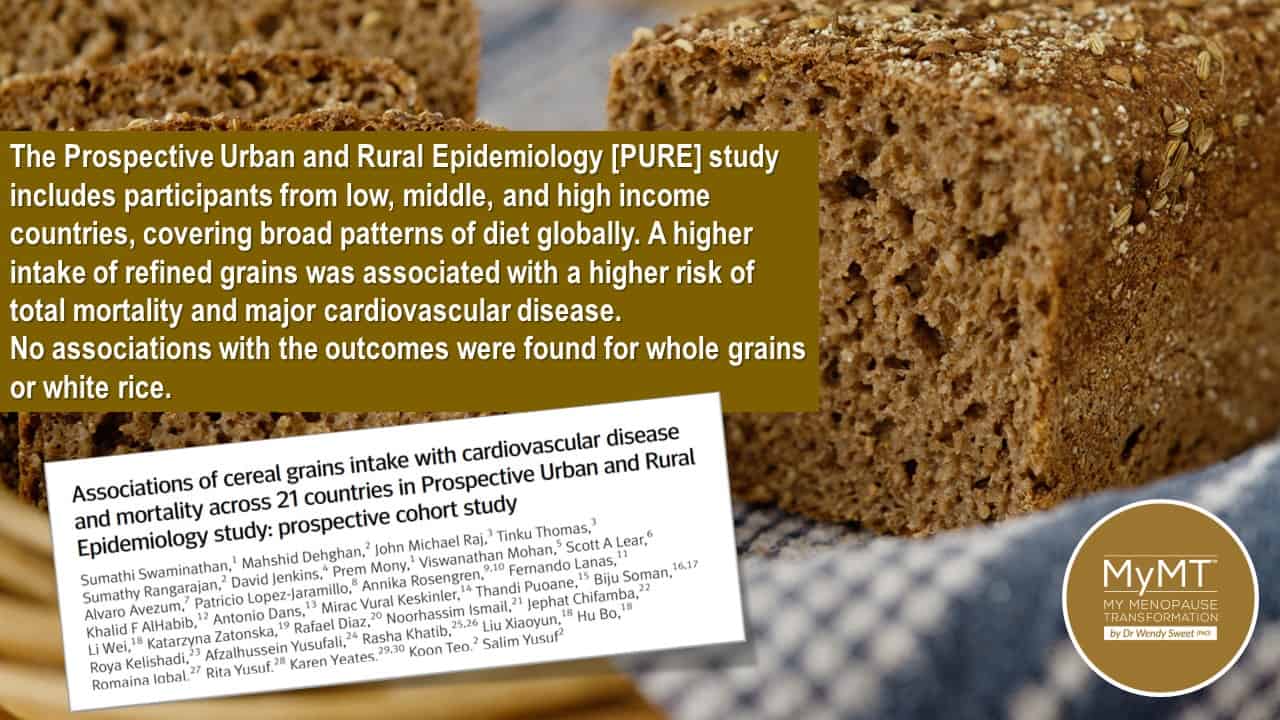
- Find foods that are low gluten or gluten-free. When it comes to anxiety and improving the reduction of inflammation, gluten proteins may contribute to leaky-gut syndrome. Whilst further research needs to be carried out on this aspect of nutrition for managing anxiety, the authors suggest that this is another nutritional strategy to implement. Rye bread has a lower gluten load and I’ve written about the importance of this type of bread for heart health during and after menopause, so finding your way with the right type of bread that might suit your inflammatory marker levels is an important step in the right direction.

- Increase Omega 3 fats in your diet. The omega 3 fatty acids offer potent anti-inflammatory properties that not only support the microbiome and white adipose tissue that contributes to inflammation, but are known to support cognition and mental health. On the practical side, this includes extra virgin olive oil, fatty fish, such as mackerel, sardines and salmon ( Alaskan sockeye salmon gets a special mention in the research, as does krill oil).

- Increase your intake of Turmeric (Curcumin). Turmeric is one of the most heavily studied spices for brain health with its active ingredient, curcumin, explored in Alzheimer’s Disease, depression, anxiety-related disorders and anxiety itself. Whilst some studies have challenged the relevance of the health benefits of Turmeric due to differences in the bioavailability of this spice in humans when taken as a supplement, on the whole, if consumed in the of food and with black pepper as well as fats, then it may have benefits for those suffering from anxiety, due to changes in inflammatory pathways.

- Ensure your Vitamin D and Vitamin B levels are adequate. In the brain, Vitamin D regulates calcium balance which in turn assists nerve-transmitter levels. It also helps with transmission of mood hormones, dopamine and serotonin. Vitamin D is also known to have benefits to the gut microbiome, because it helps to reduce inflammation. I’m often talking about Vitamin D levels for women in menopause and getting these checked, because if you are deficient in this vital hormone (yes, it is now known as a hormone), then these low levels may be contributing to your heightened feelings of anxiety.
Nutrition regulates anxiety disorders by influencing the gut microbiome and inflammation as you can see from the image below. The gut microbiome and inflammation are inter-related and therefore, work in a two-way relationship with anxiety.
This is why, for women who feel a lot of anxiety, changing nutritional approaches may be helpful. So, too may be moving towards more of a Keto dietary approach for women who are thinner and leaner.
On the MyMT™ programmes, I talk a lot about anxiety in my coaching group. I’m always reminding women that menopause per se if not the issue or the problem. All women go through this life-stage. When we stop worrying about our hormones and focus on how our body is ageing and changing as we enter our ‘third age’, then it becomes a game-changer in terms of understanding how to look after ourselves in midlife and beyond. It was for me too.
I hope you can join me sometime.
Dr Wendy Sweet (PhD)/ MyMT™ Founder/ Member: Australasian Society of Lifestyle Medicine.
References:
Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Front Psychiatry. 2018 Mar 13;9:44.
Norwitz NG, Naidoo U. Nutrition as Metabolic Treatment for Anxiety. Front Psychiatry. 2021 Feb 12;12:598119. doi: 10.3389/fpsyt.2021.
Wilcox HH. Changes in nervous system with age. Public Health Rep (1896). 1956 Dec;71(12):1179-84.