
Menopause Symptoms
Learn more about the symptoms that can be caused by menopausal hormonal changes
There is so much more to menopause symptoms than hot flashes
As you’ve reached mid-life, have you noticed a lot of changes in your body? Are you not sleeping? Do you have joint pain? Perhaps your gut health has changed? Have you experienced heart palpitations or more anxiety? Do you feel exhausted and more forgetful? Or perhaps you have gained weight or belly fat?
Menopause isn’t just about hot flushes. In perimenopause, your body goes through a variety of changes which may cause all of these symptoms and more. These may continue into post-menopause if you don’t learn how to change your lifestyle to adapt to your new hormonal environment.
Symptoms you may not know are symptoms






What causes menopause symptoms?
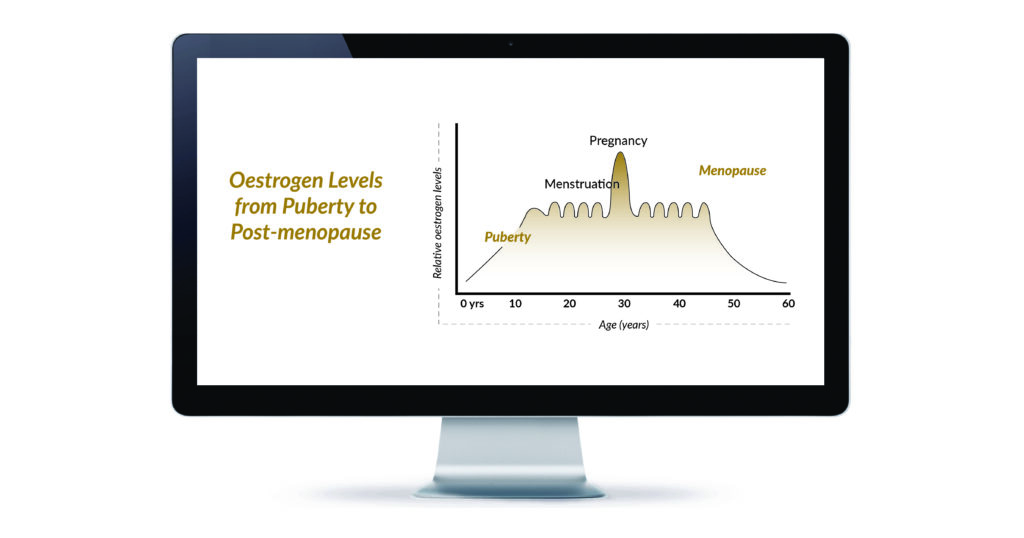
From a biological point of view, our menopause transition means that the reproductive hormones oestrogen and progesterone, as well as our master pituitary hormones, are declining. But that’s not all.
Oestrogen receptors are present around the body including in the brain, heart, breast, liver, uterus, bone, muscles, blood vessels and within the largest organ, the skin. As oestrogen levels naturally decline, these other areas of the body are affected too.
Menopause is the gateway to our biological ageing. As such, many of our main organs are reducing in size and function too. For example, did you know that the volume of the liver can reduce up to 40% during menopause and into post-menopause?
It’s no wonder so many women feel out of sorts and completely robbed of their confidence, energy and health when they reach midlife. On top of this, what we’ve done in the past to manage our health often may not work in this new hormonal environment. This is because there are so many internal factors fighting against us.

Menopause symptoms are manageable
When you reach midlife (early 40s-late 60s), your body is preparing for biological ageing and your hormonal environment changes drastically. During midlife, oestrogen and progesterone levels decline, causing a variety of symptoms.
We’ll explore the most common ones below. Whatever your menopause symptoms may be, don’t despair. There are natural, lifestyle solutions that are scientifically proven to relieve them.
The key is to work with our changing hormones, not against them.
By addressing the underlying cause of your menopause symptoms at the cellular level, not only can you experience relief from your symptoms, but you can reduce inflammation in your cells, setting you up for better health in the years to come.

Your MyMT Program is critical for all women.
I was stumbling through menopause, but it’s given me a road-map to put into action.
Cindy
Australia
When does menopause occur?
There are three distinct phases of menopause.
I often say menopause is the ‘book-end’ of puberty. It is a period in our lives when menstruation stops due to hormonal fluctuations within the ovaries and bloodstream. The average age of cessation is 48–52 years old, according to clinical studies. Western women usually stop menstruating between their mid 40s to mid 50s, unless they have a medical reason to enter premature menopause..
Source: When does Menopause occur and how long does it last?

Phase 1: Peri-menopause
Your periods begin to fluctuate, sometimes becoming irregular, lighter or heavier. Your ovaries are still producing oestrogen, but less of it as your ovarian follicles decline. The key thing to remember here, is that your ‘master reproductive hormones’, Follicle-stimulating Hormone (FSH) and Luteinising Hormone (LH) are still being produced in your pituitary gland. High FSH is associated with a range of symptoms including worsening hot flushes, poor sleep and changing cardiac health.
Phase 2: Menopause
This is when your periods cease and the average age globally is around 51-52 yrs old.
Some women go through menopause earlier or later than 51 – 52 years, and this can be due to a number of reasons such as age at menstruation, number of pregnancies, hormonal use, and your lifestyle and stress levels.
If women enter menopause before 45 years, this is considered early menopause which can herald an increased risk of chronic disease, including osteoporosis and cardiovascular disease. [Lancet, 2024]

Phase 3: Post-Menopause
When your periods have ceased for a year or more, you are now in post-menopause.
Women remain in post-menopause for the rest of their life. With life expectancy having increased dramatically over the past 100 years, women are remaining in post-menopause for longer than ever.
Some women still struggle with symptoms in post menopause or develop health issues such as cardio-vascular disease and osteoporosis. It is important for you to understand how you can change your nutrition and lifestyle to optimize your brain health, bone and muscle health and heart health to add life to your years.

How do you know if you’re in menopause?
- Do you reach for a fan when everyone else puts on a sweater or a jumper?
- Can’t remember the last time you slept 8 hours?
- Are you putting on weight and can’t work out why?
- Do you find yourself struggling with joint pain and inflammation?
- Are you feeling anxious or experiencing mood swings?
- Are you experiencing digestive issues such as bloating?
I encourage you to take my free menopause symptoms quiz if you’re not sure. You can take this quiz to find out what stage you’re at and how severe your menopausal symptoms are (in comparison to the 500,000 women who’ve already taken it).
What are common symptoms of menopause
According to over 500,000 women who took the signs of menopause quiz, hot flushes and brain fog aren’t always their top concerns. The survey results paint a different picture of menopause:
83%
The most pressing issue for women is fatigue.
81%
Struggle with sleep, which is closely linked to their fatigue.
80%
Experience sore joints that significantly impact their quality of life and activity levels.
76%
Perceive themselves as overweight.
73%
Report as being diagnosed with high blood pressure.
The A - Z of Menopause Symptoms
Below are some common menopause symptoms. There are a lot of symptoms women face during this period, but we'll cover the ones that are most troublesome.
Menopause and joint pain (880), aching joints menopause (880), sore joints menopause (880), menopause and joint aches (880)
Oestrogen plays a huge role in our joint and muscle function. So, what happens as we move through menopause, when we don’t produce as much oestrogen?
Our joints and tendons have oestrogen receptors. Prior to menopause, oestrogen helped our joints to stay supple. Higher levels of oestrogen help our collagen production, an important part of cell regeneration.
The hormone oestrogen is also responsible for our muscles’ ability to handle heavy loads and to heal and recover overnight. Oestrogen also plays a significant role in helping tocopherol (Vitamin E) and magnesium get across the joint membranes to help keep them healthy.
It makes sense then, that when oestrogen levels decline in menopause, our joint and muscle function is affected too.
Are your aching joints affecting your ability to do the things you love? Maybe your knees are stiff when you get out of bed? Or your legs feel restless and heavy? Maybe you feel dizzy and lose your balance easily, which has affected your mobility?
MyMT™ Restore your Joyful Joints is a mini course to help you relieve your aching joints
during peri-post menopause.
Learn More Below:
- www.mymenopausetransformation.com/mymt-restore-your-joyful-joints
- www.mymenopausetransformation.com/sore-joints/https-www-mymenopausetransformation-com-sore-joints-menopause-isnt-just-about-hot-flushes-discover-my-4-factors-to-help-your-sore-joints-too
- www.mymenopausetransformation.com/sore-joints/the-connection-between-your-sore-joints-and-changing-oestrogen-levels-during-menopause
- www.mymenopausetransformation.com/sore-joints/the-connection-between-your-sore-joints-and-changing-oestrogen-levels-during-menopause
Women are more likely to report high anxiety symptoms when in early or late perimenopause. In addition to our nervous system ageing and changing as our oestrogen levels decline, menopause-related anxiety may also be caused by an increase in inflammation in our cells and tissues, which includes our ageing brain and our nerves that allow us to function on a daily basis.
As our nervous system loses the role of oestrogen in the outer layer called the myelin sheath, it becomes more ‘irritable’. Chemical messages don’t get sent properly and this increased nervous-system irritability makes our heart rate speed up and we feel more anxious.
Add to this, not sleeping, too much (or too little) exercise, as well as a poor diet, and we become wired, tired, worried and anxious. For many women in mid-life, it’s not long before we experience ‘burn-out’. If we don’t allow our nervous system to calm down or give it the right nutrients, we run the risk of remaining in the ‘red zone’ of our adrenals working overtime in ‘fight and flight’ mode day after day. This spells disaster for hot flushes, depression, brain fog and of course, anxiety.
Learn More below:
- New Research: Does daily stress affect your client’s menopause symptoms?
- www.mymenopausetransformation.com/anxiety/is-your-menopause-anxiety-making-you-anxious
- www.mymenopausetransformation.com/exercise-in-menopause/walk-away-menopausal-anxiety-stress-and-depression
- Discover why your increased anxiety is not just about your changing hormones in menopause.
- New Research: Foods to improve menopause anxiety and cognition.
- Find your ‘flow’ and reduce multi-tasking to manage your anxiety levels in menopause.
Bloating is a common symptom of menopause that many women experience. It is caused by hormonal changes, particularly the decrease in oestrogen levels. This is because oestrogen plays an important role in gut lining healing and repair, but if levels of oestrogen are too high, or too low, then a condition called ‘Leaky Gut Syndrome’ may develop. This syndrome may lead to worsening brain-fog, memory problems, hot flushes and poor sleep.
‘Gender Medicine’ author, Dr Marek Glezerman, research showed that, in western countries alone, IBS is 4 times more common in women as they reach their menopause transition.
Throughout our life, and more so after puberty, oestrogen has helped to keep inflammation in our intestines at bay. It does this by keeping the mucosal cells in the gut wall tight – effectively preventing us from developing what is known as ‘leaky gut’. Furthermore, oestrogen helps our gut enzymes to work more efficiently.
Do you suffer from Irritable Bowel Syndrome (IBS)? Have you started feeling more bloated? Or do you swing between being constipated and having diarrhoea? Menopause bloating and gut health can be managed by simple lifestyle changes. Dr Wendy Sweet has developed a step-by-step scientifically-evidenced plan to restore gut health in peri-post menopause.
Learn More Below:
During menopause, many women experience symptoms like forgetfulness, fuzzy head, anxiety, and difficulty thinking clearly.
A sudden drop in oestrogen levels during menopause is associated with cognitive decline. (Hara, Waters et al, 2015).
As we already know, the female body releases a great deal of oestrogen from the ovaries. As it circulates throughout the body, it crosses the blood-brain barrier and acts on the brain’s cells. In the brain, oestrogen helps with cerebral blood flow and maintains nerve transmission. Oestrogen also operates as an anti-inflammatory agent in the brain.
As levels of oestrogen decline during menopause, this stage of life becomes a perfect storm for disruptions to our brain function and cognition. This is because brain mitochondria (where energy is produced) are affected in ways that cause inflammation.
But it’s not just changing hormone levels that disrupt mitochondrial function and lead to inflammatory changes in neurons. Age and stress (both current and past) have a long-lasting and negative impact on brain Mitochondria (Professor Sarnyai).
Inflammation in our mitochondrial cells is often caused by too much stress, resulting in a number of symptoms, including:
- fatigue
- brain fog and depression
- memory loss, lack of motivation and feeling overwhelmed
- pain and soreness in muscles
- headaches and migraines
- poor sleep
Learn More Below:
Depression affects up to 25% of women at some time in their lives. Some of it is serious. Some of it is mild. What’s known is that it affects far more women than men and perimenopause is a vulnerable time, especially if women have already experienced depression in their life and/or postpartum depression.
A decline in reproductive hormones during menopause impacts other important hormones, including serotonin.
Serotonin is one of the main hormones that affect memory, cognition, and moods in midlife. Many studies suggest oestrogen affects cognition and mood through modulation of serotonergic function (Epperson et al, 2012). As a result, oestrogen production decline may affect serotonin levels.
Serotonin production is also affected by sleep, gut health and stress. So if you’re under stress, not sleeping and experiencing menopause, bloating and other digestive issues, this too will impact your serotonin levels.
But there is another important contributing factor to menopause depression – inflammation. Inflammatory changes may also contribute to Menopause depression [Jacka et al, 2018; Mattina et al, 2019]. Inflammation arrives in mid-life, not only due to changes to the hormonal production of oestrogen and progesterone, but also as cells and tissues throughout the body change. This is even more so if women have a stressful lifestyle and aren’t sleeping. The term ‘inflammaging’ has been coined to describe the link between aging and inflammation.
It’s no wonder with all of these changes taking place , that midlife creates the perfect storm for menopause depression.
Lern More Below:
We also experience changes to our skin as oestrogen levels decline. It is common for most people to experience dry skin at some point in their lives, but none more so than during menopause. Age-related dry skin increases with menopause, which is the biological gateway to our ageing process. In their early 50s, some women experience extremely dry skin. For others, it gets ‘crinkly’ or ‘crepey’. Itching on the skin drives others insane. Others develop eczema. For many of you, dark spots are appearing more rapidly as well.
Learn More Below:
One of the greatest challenges for women as they come through menopause and into postmenopause is the fact that they don’t have enough energy. 83% of women who have taken the MyMT™ menopause symptoms quiz reported feeling tired. There have been over 500,000 women who have taken this quiz, so that’s a significant number reporting menopause fatigue. So, what happens to our energy levels as we come through menopause?
The first is that we’re losing muscle. Our muscles contain mitochondria, the powerhouse of the cell, and that’s where your energy is produced. Researchers are finding that when it comes to our metabolism, energy production, immune health repair and regeneration, our tiny mitochondria matter. As we move through menopause and age, we are losing muscle. When we lose muscle, we also lose numbers of our powerful little mitochondria.
As such, we need to be looking after these organelles that are so important to energy production. We also need to retain our mitochondria in muscle cells to help to prevent muscular weakness and loss of function as we get older as well as help our immune health.
Learn more about how you can preserve your mitochondria, and in turn your energy and immune health.
Learn More Below:
Although the link between falling oestrogen levels and migraines has been known for over 40 years, new research shows that migraines are three times more prevalent in midlife women than men of a similar age. Migraines are the second most globally disabling condition after low back pain.
Migraines occur due to a disturbance of the central nervous system, and occur more frequently due to stress. The changing nature of our blood vessels change as we lose oestrogen, and this impacts our nervous system, especially our central nervous system.
The central nervous system regulates heart rate, blood pressure, our response to stress and of course, temperature regulation. However there are lifestyle changes you can make to help reduce the frequency and severity of migraines.
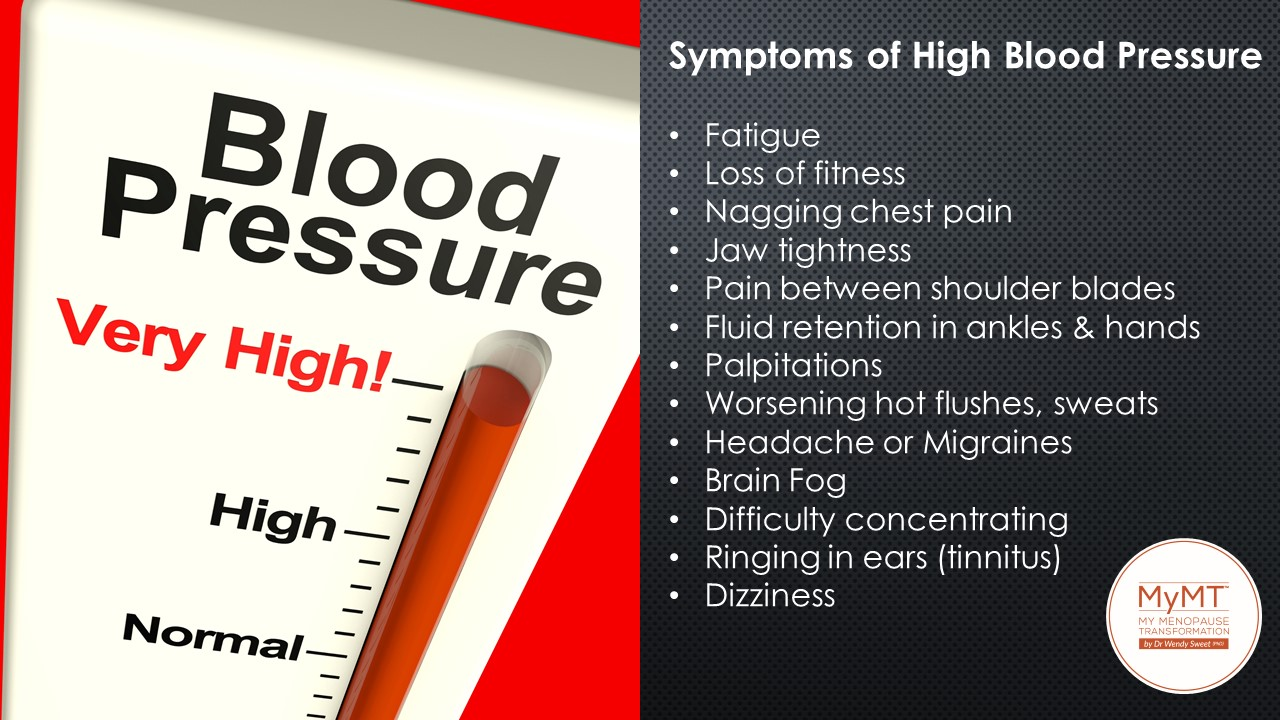
With ageing, the female heart undergoes considerable changes as oestrogen and progesterone decline.
As oestrogen naturally declines, our blood vessels lose some of their elasticity. In medical terms, it’s called vascular stiffness, and it’s very well known. This is why many women develop changing blood pressure as they come into their post menopause years.
Higher blood pressure can also contribute to hot flashes and night sweats (El Khoudary & Nasr, 2022). So if you’re experiencing hot flashes, be sure to go to your doctor to get your blood pressure checked.
Post Menopause Impacts Heart Health
With the decline in oestrogen levels as women move through menopause, risk factors for coronary heart disease (CHD) become more apparent, especially hypertension or high blood pressure.
Worldwide, 25% of adult women are hypertensive, and in the United States, more than 75% of women older than 60 years of age are hypertensive. [Lima et al., 2012]
Blood pressure risk factors during menopause
Your midlife heart health offers a critical window for implementing early intervention strategies to reduce cardiovascular risk.
The term ‘hypertension’ means high blood pressure. High blood pressure develops when blood flows through your arteries at higher-than-normal pressures. Whilst it’s absolutely normal for your blood pressure to change throughout the day based on your activities, lifestyle and dietary patterns, there are specific risk factors that are unique to women in menopause that are separate from genetic risk factors. This includes:
- history of smoking
- underlying kidney disease
- being overweight or obese
- high LDL cholesterol and low HDL cholesterol
- living a sedentary lifestyle (or doing too much exercise)
- changes to reproductive hormones which impact blood vessel elasticity
- sleep disturbance
- increased hot flushes
- alcohol consumption
- liver inflammation
- medications
Learn More Below:
- Lima, R., Wofford, M., & Reckelhoff, J. F. (2012). Hypertension in postmenopausal women. Current hypertension reports, 14(3), 254–260. doi.org/10.1007/s11906-012-0260-0
- www.mymenopausetransformation.com/blood-pressure/high-blood-pressure-in-menopause-is-this-at-the-heart-of-your-symptoms
- www.mymenopausetransformation.com/blog/from-hot-flushes-to-hypertension-getting-to-the-heart-of-the-matter-through-lifestyle-change
Hot flushes occur because the body’s thermostat does not function as well when it is deprived of oestrogen. It also becomes worse when melatonin (your sleep hormone) is impacted by your changing hormones and you aren’t sleeping. This is because there is a powerful connection between our pituitary gland in the brain, where sleep hormones are produced, our thyroid, which regulates temperature, blood pressure and metabolism, and the ovaries. Our adrenal glands are part of this connection too, which is why high levels of stress also impact hot flushes.
Normally and ideally, there is a good balance between the pituitary, thyroid and adrenal glands, where hormones are produced. However, there are numerous factors that can cause these powerful organs to get out of balance. These factors include our changing levels of reproductive hormones, our sleep quality and quantity, too much, or not enough, exercise, stress levels, the loss of elasticity of blood vessels (which increases blood pressure) and our diet, including alcohol intake.
When too much sugar or processed foods are eaten, these can have a significant impact on hot flushes. This is because, when blood glucose levels are higher than normal, the pancreas secretes a hormone called insulin. If insulin levels are high, then this can affect metabolism and temperature regulation. The result? Feelings of heat throughout the body.
Learn More Below:
- www.mymenopausetransformation.com/hot-flashes-flushes/will-my-menopause-hot-flushes-ever-stop
- www.mymenopausetransformation.com/stress/how-accumulative-stress-affects-your-sleep-anxiety-hot-flushes-and-sore-joints-in-menopause
- Your dietary protein, menopause hot flushes and the Okinawan ratio.
- Learn why your menopause weight gain, bloating and hot flushes are connected.
You may not know that you have an abundance of oestrogen receptors in your bladder and urethra. Because of this, as our oestrogen levels decline during our menopause transition, this may impact the function of the urinary tract in mid-life women.
During menopause, changes in our urinary system can present a significant challenge. One common symptom is an irritable bladder, which can lead to urgency and leakage during exercise. These changes are attributed to the decline in estrogen levels, as estrogen plays a crucial role in the function of the lower urinary tract. In addition, the loss of estrogen’s influence on the ligaments and joints can result in pelvic floor changes, contributing to stress incontinence and heightened frequency and urgency in needing to urinate.
To manage these symptoms, it is important to learn more about menopause incontinence and explore effective strategies for managing it.
Learn More Below:
MyMT™ Symptoms Quiz has been taken by over 500,000 women around the world, and 81% report symptoms of insomnia.
Wakefulness, light sleeping and insomnia (not being able to get back to sleep), is linked to changing reproductive hormones during menopause. When we don’t make lifestyle changes to accommodate these hormonal changes, sleep problems can persist.
During the transition into menopause, changing hormones levels can disrupt our normal circadian rhythms. This internal clock, which gradually becomes established during the first months of life, controls the daily ups and downs of biological patterns, including body temperature, blood pressure, and the release of hormones.
The internal clock isn’t the only thing disrupted. High insulin levels, cortisol levels, and low melatonin levels can also play havoc with sleep during the menopause transition. Other factors such as low levels of vitamin D, iron, and calcium intake can also contribute to sleep disturbances.
When we don’t get deep, restorative sleep between 2am and 4am, our immune system and overall health may suffer.
For millions of women, not sleeping during their menopause transition sends them spiraling into more health chaos as they age. Sleep is the foundation for our healthy ageing.
Not sleeping due to insomnia, night sweats, and wanting to use the bathroom, may lead to ongoing inflammation in muscles, joints, pancreas and heart. It’s partly why women end up with sore joints, aching muscles, more hot flushes and feeling bad tempered too.
Learn More Below:
Vaginal dryness is a common symptom of menopause due to the decline in oestrogen levels. As oestrogen helps maintain the lubrication, elasticity, and thickness of the vaginal walls, lower levels of oestrogen can result in thinning, drying, and inflammation. This can lead to discomfort, rritation, and pain during intercourse, making it important to address and manage this symptom during menopause.
With age, your vagina becomes less elastic, shorter and narrower and the vaginal opening becomes smaller. Oestrogen is the primary hormone that regulates the physiology of the vulvo-vaginal tissues.
Vulvovaginal atrophy refers to the specific atrophic (shrinking) changes of the vulva and vagina that occur progressively after menopause in all women. As a result of declining oestrogen, several symptoms, including vaginal dryness, irritation, and discomfort, can develop as well.
Learn More Below:
New research suggests that menopause is strongly associated with weight gain, a symptom for up to 70% of women (Kodoth et al, 2022). In fact, 73% of women who take the MyMT™ menopause symptoms quiz consider themselves overweight.
When oestrogen production begins to decline in perimenopause, the two master hormones, Luteinising Hormone and Follicle-stimulating Hormone, are still trying to send signals to the ovaries to increase production of oestrogen, but the ovarian oestrogen receptors are ageing and dying off, so the nervous and hormonal system can get out of balance.
Fat cells store additional oestrogens as we move through menopause, and the fat cells themselves produce their own oestradiol. This causes the fat cells to expand, and oestrogen can become the dominant hormone in relation to progesterone.
But fat-storage is not the only part of the menopause weight-gain story. Our liver health matters too. If the liver is fatty or inflamed, it can’t clear excess oestrogens. When our liver can’t metabolise excess oestrogens effectively, our fat cells store these additional oestrogenic compounds as we move through menopause. When women have a lot of stress in their life, or they aren’t sleeping, oestrogen can decline more rapidly and some of the signals between the brain and the ovaries get out of balance.
Learn More Below:

What are the early symptoms of menopause
Early symptoms of menopause begin with perimenopause.
What is perimenopause?
Perimenopause refers to the years leading up to actual menopause which is the point in time when permanent cessation of your menstruation occurs. Globally, the average age that you enter menopause is around 51-52 years old, unless of course, you have gone into surgical menopause after a hysterectomy or after other medical interventions. Natural peri-menopause begins around your mid-40’s, but this can change according to when you began puberty or due to the age you were when you had children.
Peri-menopause is usually the time when symptoms such as hot flushes/ flashes, dry or less elastic skin, weight gain, irregular bleeding, sore joints, anxiety, dizziness and/or feelings of depression and lethargy begin. It’s tough for many women and I had many of these symptoms too – which I found confusing and frustrating. At the time, what I didn’t realise, was that my body was ageing and in my mid-late 40’s, I wasn’t actually in menopause, but peri-menopause.
Menopause is the stage that periods stop but the years prior to that (peri-menopause) is when our hormones are fluctuating, not only within the ovaries but within our bloodstream as well.
Take control of your menopause symptoms today
For millions of women around the world, their menopause transition throws them into health and symptom chaos. But it doesn’t have to be like this at all. Menopause used to make me feel so frustrated and despondent until I began researching it.
Menopause is the biological gateway to ageing. In order to age healthily, we need to understand how to manage and/or reduce inflammation. To find out how, I explored research on women’s healthy aging and what I learnt astounded me.

Deb - Canada
“I’ve lost 25lbs (12kgs), I sleep through the night, and I can think much more clearly. The joint and muscle pain is much better. I feel like I have a life again.”

Wendy - United Kingdom
“I am just so grateful that I had something to cling to through dark times, and a community that was supportive and helpful and positive. I cannot thank Wendy enough for making this her specialism and publicising natural ways of getting through this challenging period.”

Jane - New Zealand
“After 25 years plus, with hot flushes, insomnia, depression, weight gain and countless other issues, I finally found Wendy! What a joy the past 12 weeks has been as I’ve been learning to live again!”
Symptoms vary by culture
Did you know that many cultures around the world don’t experience the same symptoms of chaos that western women do?
A large proportion of literature looking at cultural influences on menopausal experience has focused on Japan. This interest is stimulated by the fact that Japanese women are some of the healthiest in world, outliving women in the west by five years. This is why studies on Octogenarian women living on Okinawa Island, have caught my attention in women’s health and ageing studies.
With reported lower occurrences of osteoporosis, breast cancers, heart disease and reproductive cancers, as well as no word in their dictionary for hot flushes, it is easy to assume that these differences are solely due to genetic factors, however, migration studies have shown that when Japanese women move to the United States of America their prevalence of these disorders increases to a similar rate of Caucasian American women. This change in disease prevalence suggests the importance of cultural and environmental factors to the health of women.
We can learn a lot from women in different cultures. As part of my PhD studies, I seeked to understand the social, nutritional and exercise behaviours of women living with no symptoms. Many of these women live in geographical pockets around the world, known as the Blue Zones. I share powerful insights from the Blue Zones countries with you in the MyMT™ Programmes.

