It wasn’t just hot flashes and night sweats that were waking up Romany night after night – it was needing to pee as well.
I know that menopause and frequent urination affects many of you too. Before the world turned into chaos, I was traveling throughout New Zealand, Australia, and the United Kingdom sharing my live Masterclass on Menopause, and hundreds of hands would shoot up in the air when I asked who was waking up because they needed to pee in the night. Everyone laughed when they looked around the room and saw that they weren’t alone. Perhaps this is you as well.
Increased urinary frequency is a common menopause symptom. The changes to our urinary system during menopause can be such a challenge for many, not only during the night, but for those of you who experience the sudden urge to pee and some leakage when you are exercising. Our irritable bladder and urge to pee more frequently, is another symptom of menopause. However, a word of caution too – it can also be a sign of Urinary Tract Infection (UTI). Hence, if you are experiencing painful urination, or if you have any pelvic or back pain, then head to your doctor right away.
The Mystery of Bladder Issues in Menopause
Urinary urgency, urinary incontinence, increased bladder activity and reduced bladder control are all bladder symptom experiences impacted by menopause. Here’s why.
After my very anecdotal survey of hundreds of women during my live events before the pandemic, I wasn’t surprised to find that epidemiologic studies report that approximately 1 in 4 women are affected by pelvic floor and urinary tract disorders with the highest rates in menopausal women. [Wu, Vaughan et al, 2014].
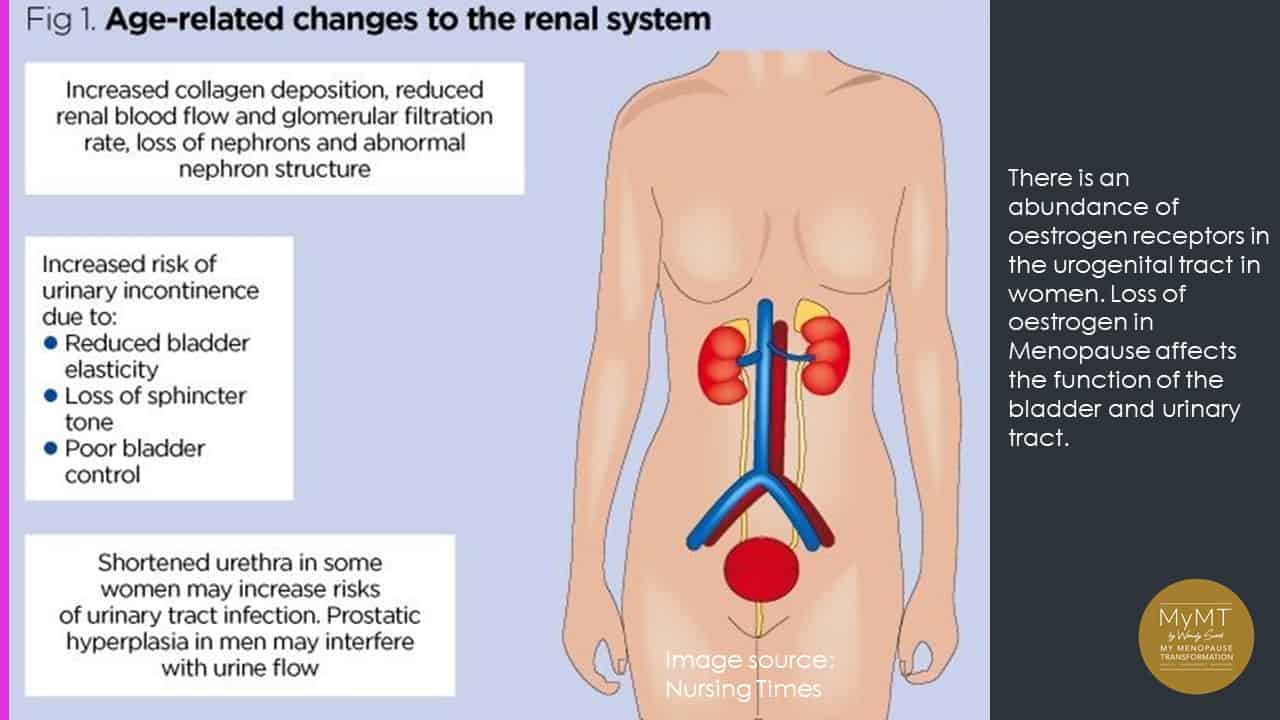
“There is clear evidence that oestrogen regulates the uro-genital tract. The abundance of estrogen receptors (ERs) in the urogenital tract explains why the natural reduction of endogenous oestrogen, the hallmark of menopause, can cause or potentiate Pelvic Floor Disorders (PFDs) and Urinary Tract Infections (UTIs).” [Alperin, Burnett et al. 2019].
The female hormone estrogen is known to have an important role in the function of the lower urinary tract throughout our life. Oestrogen and progesterone receptors demonstrate an influence in the vagina, urethra, bladder and pelvic floor musculature and like most of our organs, when we go into peri-menopause (the start of menopause) and move towards post-menopause, our renal system is experiencing the result of declining estrogen production.
You may not know that you have an abundance of oestrogen receptors in your bladder and urethra. Because of this, as estrogen levels decline during our menopause transition, this may impact the function of the urinary tract in mid-life women. Furthermore, with the loss of the role of oestrogen in our ligaments and joints, our pelvic floor changes as well. This may cause many women to experience stress incontinence and/or increased frequency and urgency in needing to pee.
Whilst it always pays to see a healthcare professional who specialises in this area, it also helps to understand what is going on and how we can help ourselves as well. So, first things first. You need to understand that your bladder and urinary tract is aging and changing.
Physiological factors that cause bladder symptoms
Age-related reduction in bladder capacity, reduced urine flow, diminished urethral pressure, and the inability of your bladder to empty fully after voiding are known changes that occur as we age. But the thing that can upset many midlife women the most is the feeling of urgency. And this is all to do with the changes that occur to the nerves that infiltrate your bladder wall. As such, stress impacts your bladder function in menopause.
Your bladder is responsive to your stress hormones, adrenaline (epinephrine), and nor-adrenaline (nor-epinephrine). This is because the sympathetic nervous system exerts influences on the urethra and bladder for urine collection and storage. Your urethra and bladder are replete with adrenergic receptors. These receptors respond to your stress hormones, adrenaline, and nor-adrenaline.
As we move into menopause and oestrogen levels decline, there is an effect on the response of the adreno-receptors in the urinary tract. Yes, they can get out of balance too resulting in an overactive bladder. This is more commonly known as ‘overactive bladder syndrome’ (OAB) or detrusor overactivity.
The term ‘detrusor’ refers to the involuntary contractions during the filling phase of the bladder that may be spontaneous or provoked and is associated with urgency. This is why the most common symptoms of OAB are urgency, nocturia (night-time urgency), frequency and urge incontinence.
As our bladder fills up and stretches, and because oestrogen levels are declining, changes also occur to the nerve signals in the bladder wall. Disruption to these nerve signals can cause nerve irritability and/or urgency and urinary incontinence. All effects which can impact on our home, working and recreational lives. I know this has occurred for many MyMT™ women, as it did for me too. Learning how to override these sensations is an important aspect of the MyMT™ programs.

How Waking Up To Pee Frequently Impacts Our Health
Night after night of getting up to have a pee is devastating for our energy. But researchers suggest that women with OAB have greater physiologic and psychologic stress reactivity than healthy controls. Importantly for women experiencing OAB, stress appears to exacerbate bladder urgency. An overactive bladder can have a huge impact on our quality of life.
When you are experiencing higher levels of stress or you aren’t sleeping well, then your chronic stress hormone called cortisol, typically increases as does your blood pressure and heart rate. Inflammation increases too and I’ve written about this numerous times in my newsletters. When cortisol is high, and there is a subsequent increase in your heart rate and blood pressure, this affects your bladder and urethra as well. Bladder control stems from the nervous system which is full of receptors that respond to stress hormones.
At night when we don’t sleep well, cortisol levels remain high, as does your blood pressure. This affects the nervous system regulation of your bladder. It’s no surprise that we feel the urge to go more frequently, especially at night. Research suggests overactive bladder symptoms affect up to 80% of women in menopause (Alperin, Burnett et al, 2019). But as I mentioned earlier, other medical conditions could be at play, such as a UTI or pelvic floor disorder. Be sure to talk to your doctor, because there are other treatment options they can discuss with you.
Pointers For Improving Menopause Bladder Control
So, what can I do about it? Here are my 5 pointers to help you:
- Re-address stress. Knowing that cortisol impacts your nervous system, especially your fight or flight nerves, and that your menopause changes impact on your nervous system, it pays to reflect on your stress levels. It is well known that anxiety increases in menopause, but again, this is also related to our changing oestrogen levels and the effect they exert on the nervous system, causing greater irritability of your nerves, including the nerves that sit within your bladder and urethra.
- Re-train your over-active nerves through relaxation exercises. Bladder retraining is hard to do, especially if you are experiencing urgency, but if your urgency isn’t to do with any bladder infection, then start to re-train it. When you feel the ‘urge’, then try to over-ride it with relaxation strategies and regular breathing through your nose. This will calm down your ‘fight or flight’ sympathetic nervous system. It may take a bit of time to do this, but as I say to women on the MyMT™ programmes, “your brain controls everything and in menopause, it just needs some re-programming now and again.”

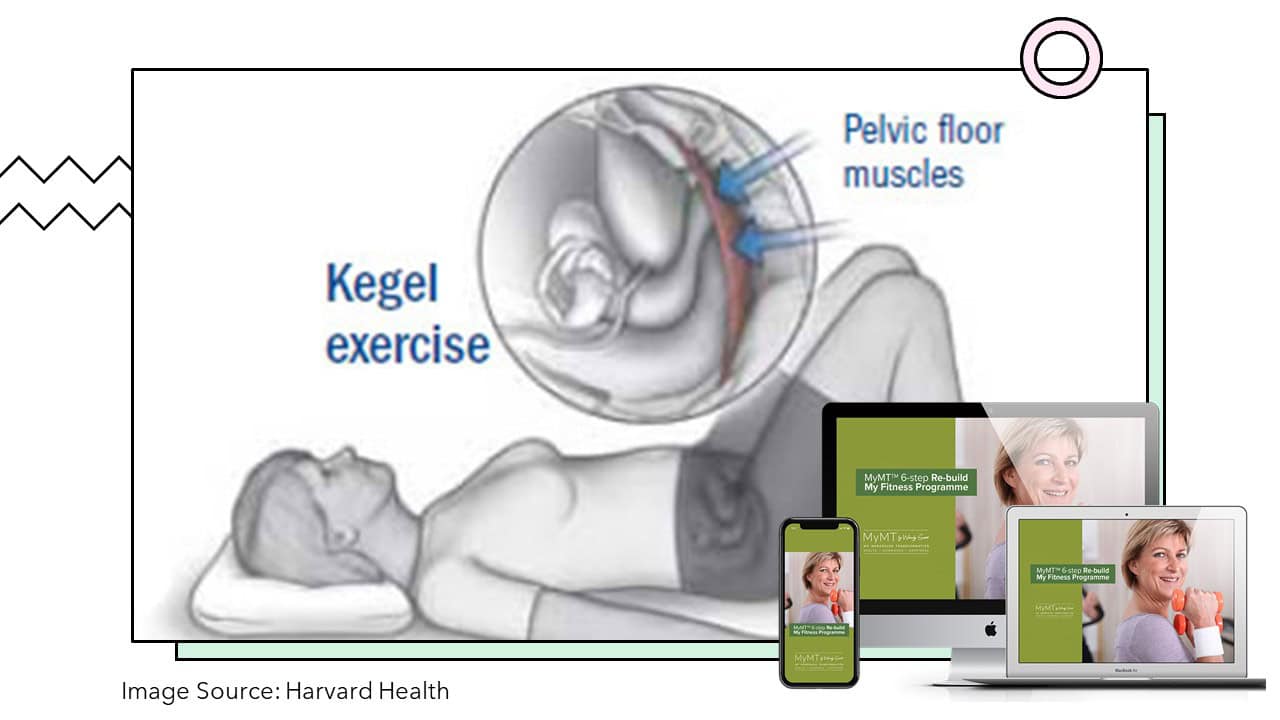
- Don’t forget your Kegel Exercises to strengthen your pelvic floor. There’s so much going on in our lives and it’s easy to forget that menopause is a time to seek professional support with your pelvic floor. Pelvic floor exercises (specifically Kegel exercises), involve squeezing and releasing your pelvic floor muscles in a timely manner. These assist in re-training the muscles that help to hold your pelvic floor in place. These muscles also lose the role of oestrogen and their loss of elasticity can cause some prolapse of your uterus or back pain from your shifting pelvis. I have Kegel exercises in my Rebuild My Fitness programme, but for those of you who can’t make it onto the programmes, then do get professional advice on the correct technique for these.
- Practice emptying your bladder completely. The knowledge that our bladder undergoes changes in the bladder wall which affects its contractility means that when we do go to the loo, there tends to be some residual urine left in there. This can also make us more prone to UTIs, so practice emptying your bladder completely on urination.
- Follow an anti-inflammatory diet. On the MyMT™ programmes, I show clear evidence as to the importance of following an anti-inflammatory diet during our menopause transition. As such I have modified the Mediterranean Diet to better suit women’s healthy ageing. Age-related inflammatory changes occur throughout the menopause transition and can worsen during post-menopause if action isn’t taken to change our lifestyle. Known as ‘inflammaging’ if you are eating the wrong food, if you are doing lots of exercise, if you are overweight or obese, and if you aren’t sleeping, then these factors are known to contribute to worsening inflammation in our body. Hence, one of the strategies to reduce cortisol levels (apart from re-learning how to sleep all night which I focus you on in the programmes) is to follow an anti-inflammatory diet. This will help reduce the inflammation that can cause bladder disruption as well.

If you’re struggling with OAB symptoms, then please get it checked out from Specialists in your area when you can. Then if you aren’t sleeping or you are feeling overwhelmed and frustrated with your symptoms, I invite you to join me in either of the 12 week MyMT™ programmes. You will be amazed at what you learn and how simple changes to our lifestyle can turn around menopause symptoms. I hope that you can spend a few minutes reading some of the wonderful stories from women who have kindly shared their journey with you on the Success Stories page on the website.

Alperin, M., Burnett, L., Lukacz, E., & Brubaker, L. (2019). The mysteries of menopause and urogynecologic health: clinical and scientific gaps. Menopause (New York, N.Y.), 26(1), 103–111. https://doi.org/10.1097/GME.0000000000001209
Harvard Health (2013). Overcoming an overactive bladder. Harvard Health Publishing Online.
Siroky, M.B. (2004). The Aging Bladder. Reviews in Urology, 6(1), 53-57.
Wu, J., Vaughan, C., Goode, P., et al (2014). Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet. Gynecol. 123, 141 – 148. [PubMed: 24463674].

