With the possible exception of pilot whales and chimpanzees, no mammals studied to date are known to commonly exhibit the cessation of their reproductive capacity as they get older.
Except of course, for human females.
For those of you with clients approaching mid-life (45-60 years), my theme this month is about ‘New Beginnings‘. That’s why I want to share this article with you. As I discovered myself when I reached my early 50s, I realised I didn’t fully understand what menopause was, nor in an in-depth way that allowed me to fully appreciate that hormonal shifts are not ‘just’ the issue for women – there is so much more going on.
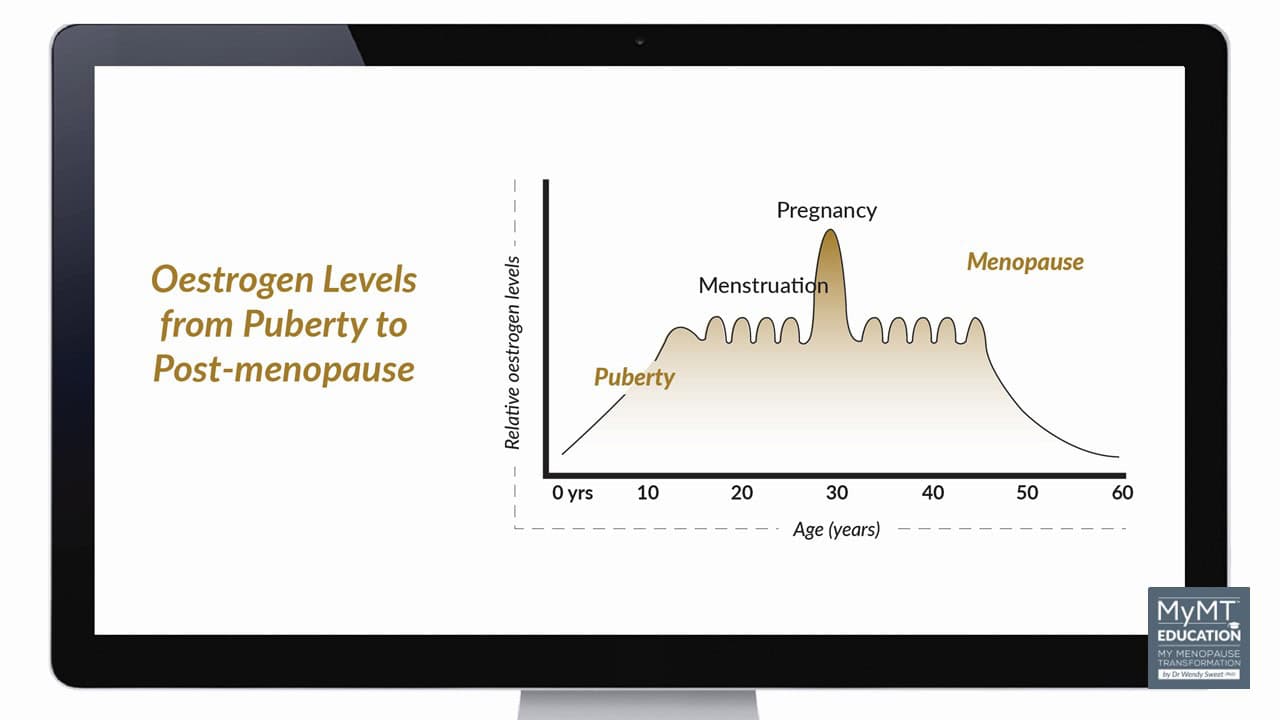
Nor did I realise that whilst the term ‘menopause’ gets thrown around as if it sums up the entirety of the change in reproductive hormones, just the same as the term ‘puberty’ does too.
But ‘menopause’ is only one stage that women transition through, there are other stages which elicit huge shifts in their physiology, as the transition from the reproductive years towards our non-reproductive years occurs.
These three stages are:
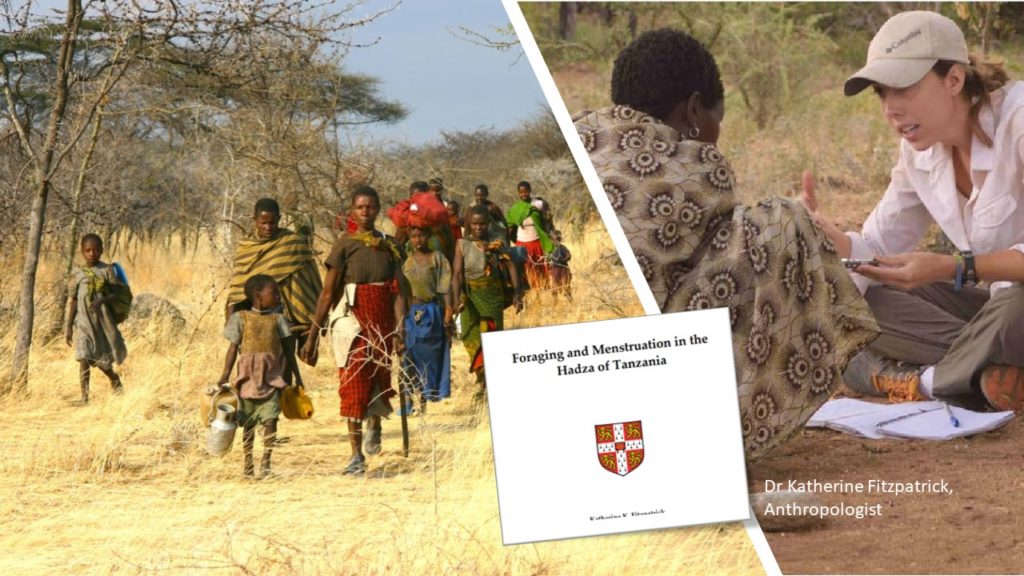
- Peri-menopause: this is when oestrogen production begins to decline as ovarian receptors for oestrogen start to die off. In most women, this begins around 45 yrs, but interestingly, in the Hadza tribal women, the average age of peri-menopause is only 40 – 41 years (Fitzpatrick, 2015).
In peri-menopause, periods still occur but may fluctuate from light to heavy, or even disappear and re-appear, which depends on numerous factors including stress, over-exercising, weight gain or other health concerns.
- Menopause: This is when periods cease. The average age globally is 51-52 years.
- Post-Menopause: When menstrual periods have ceased for a year, women enter post-menopause. This is where they remain for the rest of their life. The body has biologically aged.
I hope that sharing this article with you might help you to make sense of symptoms for your midlife clients, as they navigate this life-stage. For millions of women around the world, the menopause transition, can throw them into emotional and physical chaos.
Some women will have symptoms right from peri-menopause to post-menopause – sometimes lasting for 10 or more years, and become confused as to why many of the medications and supplements may not be working for them.
But here’s the thing.
Menopause is relatively unique to us as a species. And 100 years ago, it might not have been a problem, simply because we didn’t live very long. With 1 billion women projected to be in menopause by 2025, the world is facing a situation without precedent – we are living longer in post-menopause than ever before.
Menopause is the biological gateway towards ageing
The long post-reproductive life span of women appears to be an evolutionary trait of long standing suggests Pollycove et al (2011), in their article on the evolutionary origin and significance of Menopause.
It was this article that piqued my interest in positioning the menopause transition in ageing science for women.
From a physiological perspective, natural menopause (as opposed to surgical menopause), is when the ovaries are going into decline. As such, the ovaries no longer produce oestrogen.
In most western countries, the average age of menopause begins around the mid-40’s (called peri-menopause) and ends when women haven’t had a period for a year or more (called post-menopause). In many societies, women reach post-menopause around their mid-50’s.
Menopause is not seen as a disease, but as a survival advantage
Several theories have been proposed to explain why menopause might have evolved and efforts to understand this biological event have engaged anthropologists and evolutionary biologists for decades.
Many of these theories are based on aspects of the human life history whereby menopause is seen not as a disease, but as a survival advantage.
A doctoral thesis by Swedish researcher, Fanny Hägg, explains,
“Menopause, the cessation of female reproduction well before death, is a puzzling phenomenon, because evolutionary theory suggests there should be no selection for survival when reproduction has ended. The evolution of menopause is a complex issue, containing many factors, kinship dynamics among the most important. Theories apply unequally to various species and populations, meaning an integrated approach is necessary for decrypting the evolution of menopause. (Hagg, 2020).
Understanding what menopause represents to us as a species is important – especially if we are going to make any sense of symptoms.
Numerous theories abound, and one of these theories is known as the Adaptive Theory.
This theory is also known as the ‘Grandmother Hypothesis‘ and is the most acknowledged evolutionary theory of why some mammals (but not all) transition through menopause.
It views ovarian failure and menopause in older human females as favouring survival of their daughters, in order to help them raise and survive additional offspring.
As Hawkes et al, (1998) suggest, “Long post-menopausal lifespans distinguish humans from all other primates. This pattern may have evolved with mother-child food sharing, a practice that allowed aging females to enhance their daughters’ fertility, thereby increasing selection against senescence.”

Anthropologists believe that because human babies are incapable of moving around on their own soon after being born, and human babies need to be fed and nourished, then menopause has become a survival adaptation.
Post-reproductive grandmothers who don’t reproduce any more themselves, can therefore, assist their adult daughters. That’s why this theory is also known as the ‘Grandmother Theory’.
In the grandmother hypothesis, females can gain benefits from stopping reproduction long before they die by helping to care for their existing children (or grandchildren), instead of producing more, which helps their descendants to survive.
‘Natural selection would favour females who become infertile many years before death if offspring require exceptional duration and intensity of parental care, as is the case with humans’ suggests the authors (Pollycove et al. 2011, p. 2).

Then there is the theory that childbearing at older ages is relatively risky. There may be little advantage for an older mother in running the increased risk of a further pregnancy when existing offspring depend critically on her survival.
I do tend to agree with this one. Bringing up very young children in our 50’s and trying to cope with not sleeping and other symptoms during menopause may be very challenging, as many women are finding.
Why menopause may have evolved has been debated for decades. But researchers do tend to agree, that this stage of life confers some advantages toward survival. Not only for older women, but for daughters and grand-children. They also agree on something else to do with menopause.
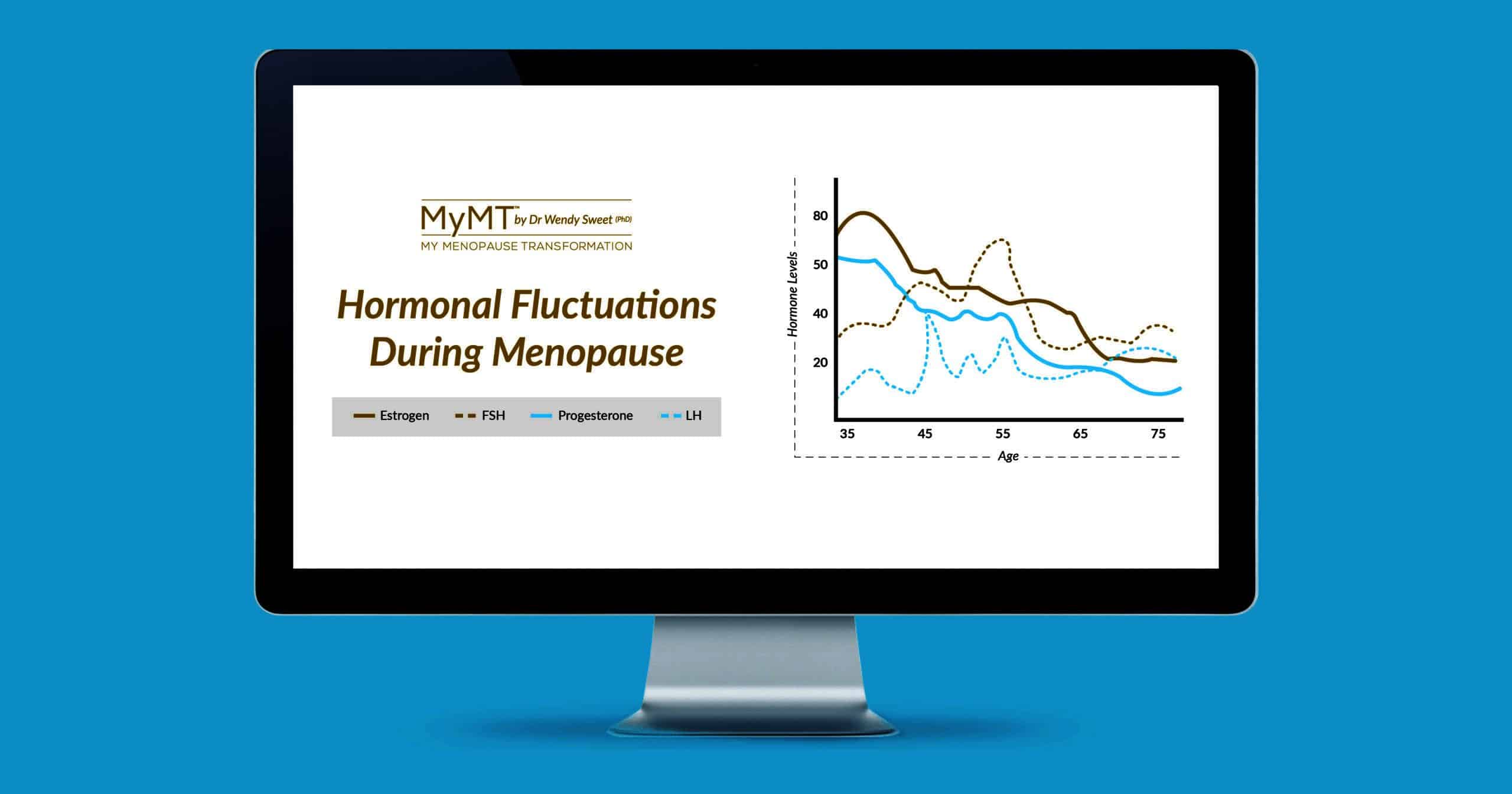
The stage of life when reproductive hormone production is reduced, accelerates ageing and advances disease risks due to an increase in inflammatory changes over time.
It’s why I always say that “menopause isn’t just about hot flushes” – there is so much more going on in this life stage, than many women are led to believe.
This is also the conclusion I came to as I did my Thesis on women’s health and ageing. Menopause is the biological gateway to ageing. It is the opposite life-stage to puberty.
Which is why I’ve situated the My Menopause Transformation Education courses within ageing research. Or should I say, ‘healthy ageing research’! Not all ageing is healthy and many disorders of older age are now linked to shifts in inflammatory changes at certain stages of mid-life. [Shen et al, Nature, 2024]
This is why a relatively new term, describing the chronic inflammatory changes due to age, is known as ‘inflammaging.’
Inflammation may make menopause symptoms worse
The term ‘inflammaging’ refers to chronic, low-grade inflammation that characterizes ageing. And as I keep reminding women, even though we feel relatively young perhaps compared to our mother’s generation, we must also remember that inside our body, cells are ageing.
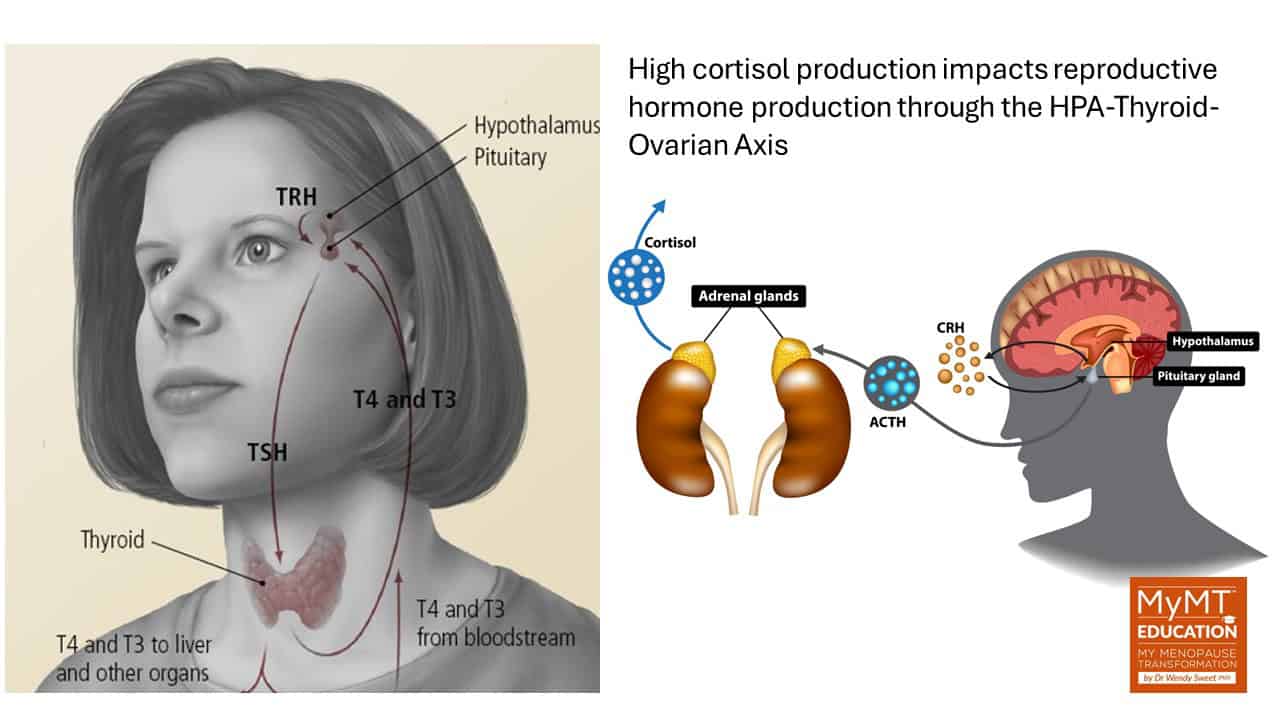
Furthermore, when women aren’t sleeping, they aren’t healing from all the stress that they may be experiencing.
And I don’t just mean emotional stress. If women are undertaking lots of high-intensity exercise throughout their week (as I used to as well), this may increase physical or oxidative stress inside cells and tissues when insomnia is present.
Like over-trained athletes, women then fail to heal properly without the benefits of deeper REM sleep. Inflammation builds up and this begins to affect several tissues and organs, including the gut microbiota and fat cells.

When inflammation is higher than normal, the chronic stress hormone called cortisol, remains higher than it should and this impacts the relative stability of the HPA-Thyroid Axis.
When cortisol is high in the body, this causes even more inflammation. And I talk about why this is, in my ONLINE Masterclass on Menopause webinar which if you aren’t quite ready for one of the certified MyMT™ Education courses just yet.
In the Masterclass I talk to you about the link between cortisol and the sleep hormone melatonin. If cortisol is high at night, then it interferes with the production and secretion of melatonin.
Without enough melatonin being produced during menopause, your midlife clients may toss and turn all night or they remain awake from around 3am.
There’s also another anomaly that scientists are learning about menopause and this is, that women haven’t evolved to live long lives.
In the pre-agriculture, hunter-gatherer period, life expectancy was around 65 yrs or less. Hence, women didn’t have to concern themselves with either menopause or post-menopause.
Today, human health and longevity has made great strides!
Many of us have watched our mother’s generation age with all sorts of ailments and functional disabilities. I remember my own mother going on “heart pills’ probably in her late-50’s or early 60’s and complaining about knees and ankles that were continually swollen and sore.
A knee replacement helped, but her activity slowed and the weight went on and her health was never the same.

Menopause is derived from the Latin words “meno” which means ‘months’ and “pausia” which means ‘halt’ respectively.
But whilst Menopause marks the end of a woman’s period of natural fertility, it doesn’t mean that women can’t feel healthy and happy as they age. This is what I focus you on understanding in the MyMT™ Education courses.
If you are going to help your clients to help themselves with lifestyle changes that I’ve researched specific to each phase of the menopause transition, then please join me sometime.
Paleontologists who study the evolution of menopause report that female hunter-gatherers remain generally active through their late menopause years and are therefore, least likely to be bothered by menopause symptoms. This was evidenced by data on sleep disorders in women from less developed nations as compared with sedentary women in post-industrial countries (Pollycove et al, 2012).
Furthermore, in more recent research, studies into the habits and physical activity patterns of women from the Hadza hunter-gatherer tribe in Africa, also found that menopause symptoms (measured as hot flushes), were low and this was partly attributed to the fact that on average, women walked 6-8km a day.
I talk about this research in my health professional courses. It’s an important starting point for you to know if you are an exercise professional too, and this is, ‘how much exercise is enough to mitigate menopause symptoms?’
For millions of women around the world, their menopause transition throws them into health and symptom chaos and many rely on Practitioners to have the lifestyle solutions for them. This came through very clearly in my own studies.
Many symptoms are being viewed in isolation, but this is not how the body works is it? That’s why, I have developed these courses for you.
For those of you who are Health Professionals, in the menopause qualifications, I dive much deeper into the science behind the 12-week programmes, and introduce you to the incredible research about behaviour change strategies specific to midlife women. My video about the 12 week Practitioner course is also below.
No matter where you are in the world and what is going on with your busy professional life, thank you for being here with me and staying curious about ‘new beginnings’ for your female midlife clients.
References:
Arbuckle, K. (2016). Why do women go through menopause? Science offers new solution to old puzzle. The Conversation.
Austad S. (1994). Menopause: an evolutionary perspective. Exp Gerontol. 29(3-4):255‐263. doi:10.1016/0531-5565(94)90005-1
Hagg, F. (2020). Evolutionary theories of menopause. Thesis: Linköping University, Sweden.
Pollycove R, Naftolin F, Simon JA. The evolutionary origin and significance of menopause. Menopause. 2011;18(3):336‐342. doi:10.1097/gme.0b013e3181ed957a
Shanley D., Kirkwood T. (2001). Evolution of the human menopause. Bioessays. 23(3):282‐287. doi:10.1002/1521-1878(200103)23:3<282::AID-BIES1038>3.0.CO;2-9
Shen, X., Wang, C., Zhou, X. et al. Nonlinear dynamics of multi-omics profiles during human aging. Nat Aging (2024). https://doi.org/10.1038/s43587-024-00692-2
Takahashi, M., Singh, R. S., & Stone, J. (2017). A Theory for the Origin of Human Menopause. Frontiers in genetics, 7, 222. https://doi.org/10.3389/fgene.2016.00222